Shoulder pain is primarily caused by rotator cuff tendinopathy, adhesive capsulitis (frozen shoulder), osteoarthritis, or instability. While most cases stem from local soft tissue inflammation, referred pain from the cervical spine (neck) or heart can also manifest as shoulder discomfort, requiring differential diagnosis based on symptom patterns
So what causes shoulder pain?
It often involves more than one structure. Muscles, tendons, the upper arm bone, or even the shoulder blade can all play a role. Sometimes the real issue comes from your neck or another nearby area.
In this article, you will learn about the main causes of shoulder pain, including:
-
Rotator cuff injuries and tendon problems
-
Frozen shoulder (adhesive capsulitis)
-
Shoulder arthritis and joint degeneration
-
Shoulder instability and dislocation
-
Acute injuries such as fractures and labral tears
-
Referred pain from the neck, heart, or other organs
-
When to seek urgent medical care
-
Treatment options and prevention strategies
Whether you're dealing with mild shoulder pain or something more severe, you'll learn what to do and when to seek help.
Everything is based on trusted clinical evidence to help you make confident choices for your recovery.
Key Takeaways
-
Most shoulder pain stems from a handful of common problems: rotator cuff injuries, frozen shoulder, arthritis, instability or dislocation, and referred pain from the neck or heart.
-
Sudden severe pain after trauma, visible deformity, fever, or shoulder pain combined with chest symptoms can signal a medical emergency requiring same-day care.
-
The pattern of your symptoms, night pain, progressive stiffness, clicking, weakness, or history of injury, often points to the likely cause more reliably than any single test.
-
Many causes of shoulder pain improve with conservative care including activity modification, exercises, medication, and physical therapy within weeks to months.
-
Persistent pain lasting more than 4–6 weeks, or pain that keeps worsening, warrants evaluation by a healthcare provider to prevent long-term problems.
How Does Shoulder Anatomy Contribute to Pain and Injury?
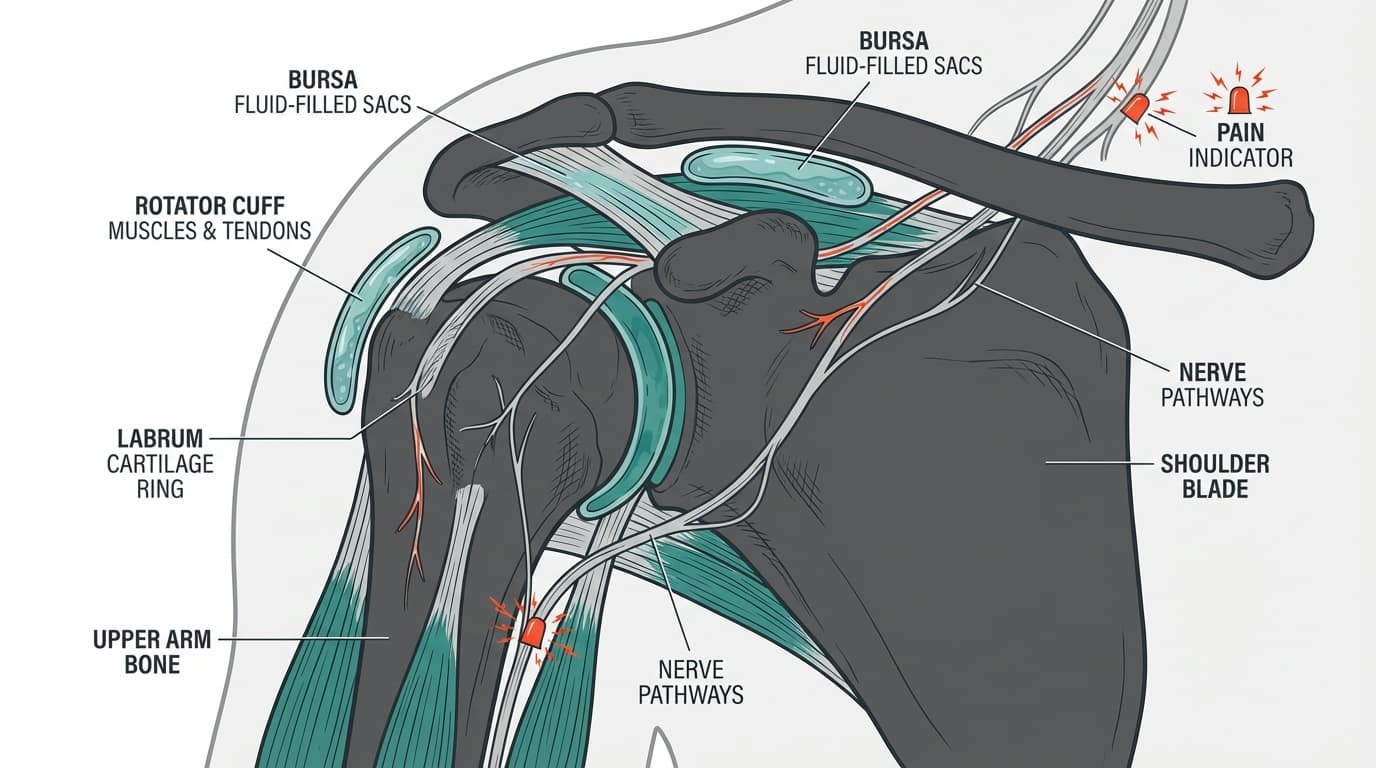
Your shoulder is built for a wide range of motion, but that flexibility comes with trade-offs. Unlike more stable joints, your shoulder relies heavily on soft tissues for support.
Here’s a quick look at the main structures that can end up causing pain:
-
Shoulder joint: Where your upper arm bone meets your shoulder blade
-
Rotator cuff: A group of muscles and tendons that keep your shoulder stable during movement
-
Labrum: A cartilage ring that deepens the socket
-
Bursa: Small fluid-filled sacs that reduce friction
-
Nerves: Can become compressed or irritated, leading to radiating or sharp pain
Because these parts work so closely together, even a mild issue in one area can create a ripple effect. That’s why shoulder blade pain, stiffness, or reduced range of motion often shares overlapping causes.
Understanding how your shoulder is built helps explain why treating pain sometimes requires more than just rest or nonsteroidal anti-inflammatory drugs.
What Are the Most Common Causes of Shoulder Pain?
Many cases of shoulder pain come down to a few common conditions that affect the muscles, tendons, joints, or soft tissues in and around the shoulder joint. Understanding these can help you recognize patterns in your symptoms and feel more confident about what recovery may look like.
Let’s walk through the most common causes and what usually helps.
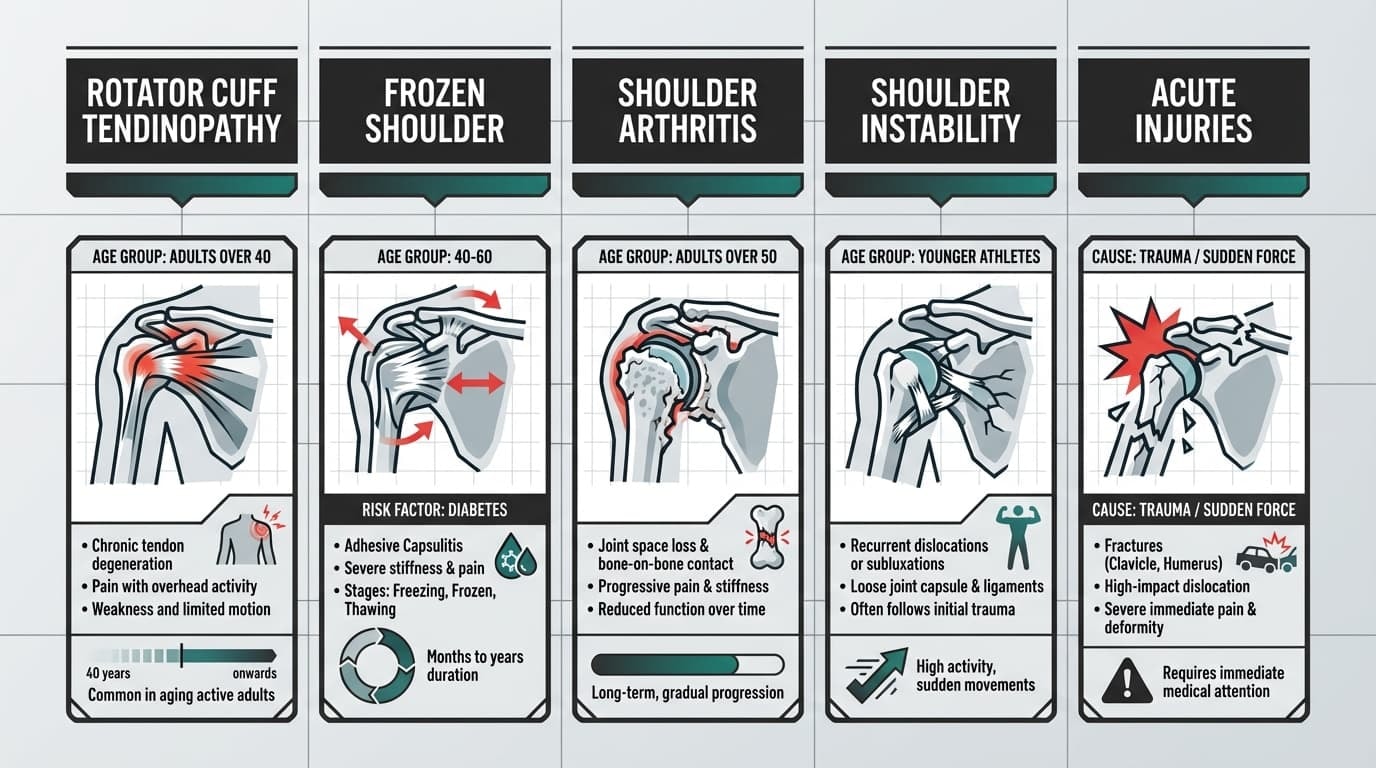
Rotator Cuff Tendinopathy and Tears
The rotator cuff is a complex of four muscles (supraspinatus, infraspinatus, teres minor, subscapularis) that stabilizes the humeral head. According to Mayo Clinic data, rotator cuff tendinopathy is the leading cause of shoulder pain in adults over 40, often caused by repetitive overhead stress.
Common in: Adults over 40, overhead workers, and athletes like swimmers, tennis players, or pitchers.
Symptoms often include:
-
Lateral Deltoid Pain: Aching pain along the outer arm caused by referred signals from the supraspinatus tendon.
-
Painful Arc: Sharp pain when lifting the arm between 60–120 degrees, indicating subacromial impingement.
-
Nocturnal Pain: Increased discomfort when lying on the affected side due to direct compression of the inflamed bursa.
What helps:
-
Temporary activity changes to avoid overhead strain
-
Strengthening exercises, especially for the rotator cuff and shoulder blade muscles
-
Physical therapy
-
Anti-inflammatory medication, if appropriate
-
Limited corticosteroid injections when needed
Most people see meaningful progress in 6 to 12 weeks with a structured rehab plan.
For added comfort during recovery, many people benefit from wearing a supportive brace that offloads pressure and keeps the shoulder in a more neutral position during daily tasks.
For mechanical offloading, clinicians often recommend a supportive compression brace like the Anaconda Shoulder Brace to maintain neutral joint alignment and reduce strain on the supraspinatus tendon during tissue repair.
Frozen Shoulder (Adhesive Capsulitis)
Frozen shoulder, clinically known as adhesive capsulitis, is a condition where the glenohumeral joint capsule thickens and contracts, severely restricting active and passive range of motion.
This condition disproportionately affects adults aged 40 to 60, particularly those with systemic comorbidities like diabetes or thyroid disorders.
Common in: Adults between 40 and 60, especially those with diabetes or thyroid issues.
Symptoms often include:
-
Gradual onset of pain and stiffness
-
Difficulty with both active and passive movement
-
Worse at night or during sleep
-
Clear limitation in external rotation, even when someone else tries to move your arm
What helps:
-
Long-term mobility-focused physical therapy
-
Pain relief strategies, including medication or occasional joint injections
-
Gentle stretching and home exercises
-
Patience — recovery often takes 1 to 3 years
During the early painful stages, a shoulder brace like the Anaconda can offer comfort and support, allowing you to go about daily life while minimizing further strain.
Shoulder Arthritis (Glenohumeral and AC Joint)
Shoulder arthritis occurs when mechanical wear or autoimmune inflammation degrades the hyaline cartilage cushioning the glenohumeral or acromioclavicular (AC) joints.
Common in: Adults over 50, especially those with prior injuries, repetitive overhead work, or inflammatory conditions.
Symptoms often include:
-
Deep, aching joint pain
-
Stiffness that worsens over the years
-
Grinding or clicking with movement
-
Difficulty with the full range of motion
What helps:
-
Mobility and strength exercises
-
Nonsteroidal anti-inflammatory drugs
-
Injections for more advanced cases
-
Joint replacement surgery if conservative treatments no longer help
Shoulder Instability or Dislocation
This occurs when the upper arm bone slips partially or completely out of the socket, usually from trauma. It may lead to repeated episodes of instability.
Common in: Younger, active individuals, especially in contact sports.
Symptoms often include:
-
Sudden sharp pain during the injury
-
Weakness or “giving out” during certain motions
-
Apprehension with overhead or reaching movements
-
Recurring dislocations
What helps:
-
Immediate reduction of a full dislocation
-
Short-term sling use
-
Rehab to strengthen the shoulder stabilizers
-
Surgery for repeated instability or labral damage
Acute Injuries (Fractures, Tears, Calcific Tendinopathy)
Sudden shoulder pain, especially after a fall or accident, may signal a fracture, tendon tear, or inflammation from calcium deposits.
Common in: People of any age after significant trauma, or those with undiagnosed tendon wear.
Symptoms often include:
-
Intense, sharp pain
-
Visible swelling or bruising
-
Difficulty moving the arm normally
-
Pain that does not match typical overuse patterns
What helps:
-
Emergency care and imaging (X-rays or MRI)
-
Pain management
-
Early surgical review for large rotator cuff tears or misaligned fractures
-
Gradual return to movement under guidance
Referred Shoulder Pain: When the Problem Isn’t in the Shoulder
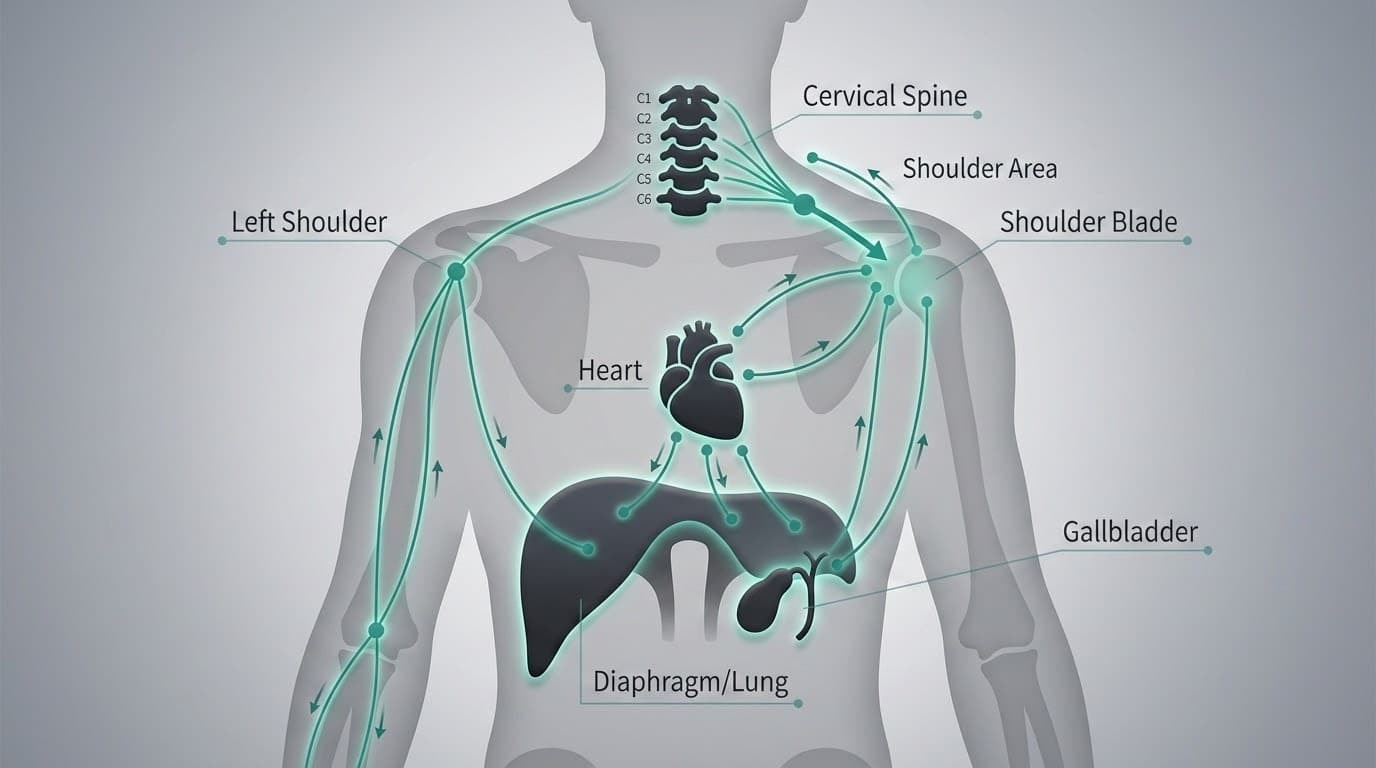
Not all shoulder pain starts in the shoulder. Sometimes, discomfort in the shoulder, shoulder blade, or upper arm is actually coming from another part of your body. This is called referred pain, and it happens because nerves in different areas share similar pathways.
Recognizing referred pain is important because treating the shoulder directly won't help if the real problem is somewhere else.
Let’s take a closer look at the most common sources of referred shoulder pain and how to tell them apart.
Neck-Related Shoulder Pain
The neck, or cervical spine, contains nerves that travel down the shoulder and into the arm. If these nerves are irritated or compressed, the pain can feel like it's coming from the shoulder even though the joint is healthy.
You may notice:
-
Pain that radiates past the shoulder to the elbow or fingers
-
Tingling, numbness, or a pins-and-needles sensation
-
Pain that changes with head or neck movements
-
Shoulder pain that does not get worse with shoulder motion itself
If moving your neck affects your shoulder pain more than moving your arm, the source may be your neck.
Heart-Related Shoulder Pain
Pain in the left shoulder or arm can be a warning sign of a heart problem, especially if it comes with other symptoms.
Call emergency services if you have:
-
Chest discomfort with pressure or tightness
-
Pain that spreads to your jaw, left arm, or back
-
Shortness of breath, nausea, or cold sweats
-
Pain that starts during activity or emotional stress
Cardiac-referred pain typically presents as angina—a deep, crushing pressure radiating to the left shoulder, jaw, or neck via the phrenic nerve pathway, and notably does not worsen with shoulder palpation or movement.
Gallbladder Pain Referred to the Shoulder
The gallbladder can cause referred pain to the right shoulder or shoulder blade, especially when inflamed or blocked by gallstones.
You might experience:
-
Pain in the upper right abdomen after eating fatty meals
-
Nausea or bloating
-
Discomfort that radiates to the right shoulder or upper back
Digestive symptoms along with shoulder pain are a clue that the issue may be internal rather than joint-related.
Diaphragm or Lung Causes
The diaphragm sits just below your lungs and shares nerve pathways with the shoulders. Lung problems can also cause pain in the shoulder or upper back, especially near the shoulder blades.
Look out for:
-
Shoulder pain that worsens with deep breaths or coughing
-
Breathing difficulty or a recent chest illness
-
No clear connection between pain and shoulder movement
If you have recent chest trauma, respiratory symptoms, or abdominal surgery and now feel unexplained shoulder or shoulder blade pain, the cause may lie deeper.
How to Tell If Pain Is Referred
Referred pain can be tricky, but here are some signs to watch for:
-
Pain that does not change with shoulder movement
-
A deep, hard-to-pinpoint ache
-
No improvement with standard shoulder treatments
-
Other symptoms like nausea, fever, or chest tightness
On the other hand, pain coming from the shoulder joint itself usually:
-
Gets worse when you move the shoulder or arm
-
Is sharp or achy during specific activities
-
Responds to rest, ice, or physical therapy
When Referred Pain Is a Red Flag
Some types of referred pain are harmless, but others are signs of serious conditions. Seek urgent care if you notice:
-
Shoulder pain with chest pressure or difficulty breathing
-
Pain after trauma with visible deformity
-
Redness, heat, and fever near the shoulder
-
Weakness or numbness in the arm or hand
-
Sudden inability to move the shoulder after an injury
Red-Flag Shoulder Pain: When to Seek Urgent Care
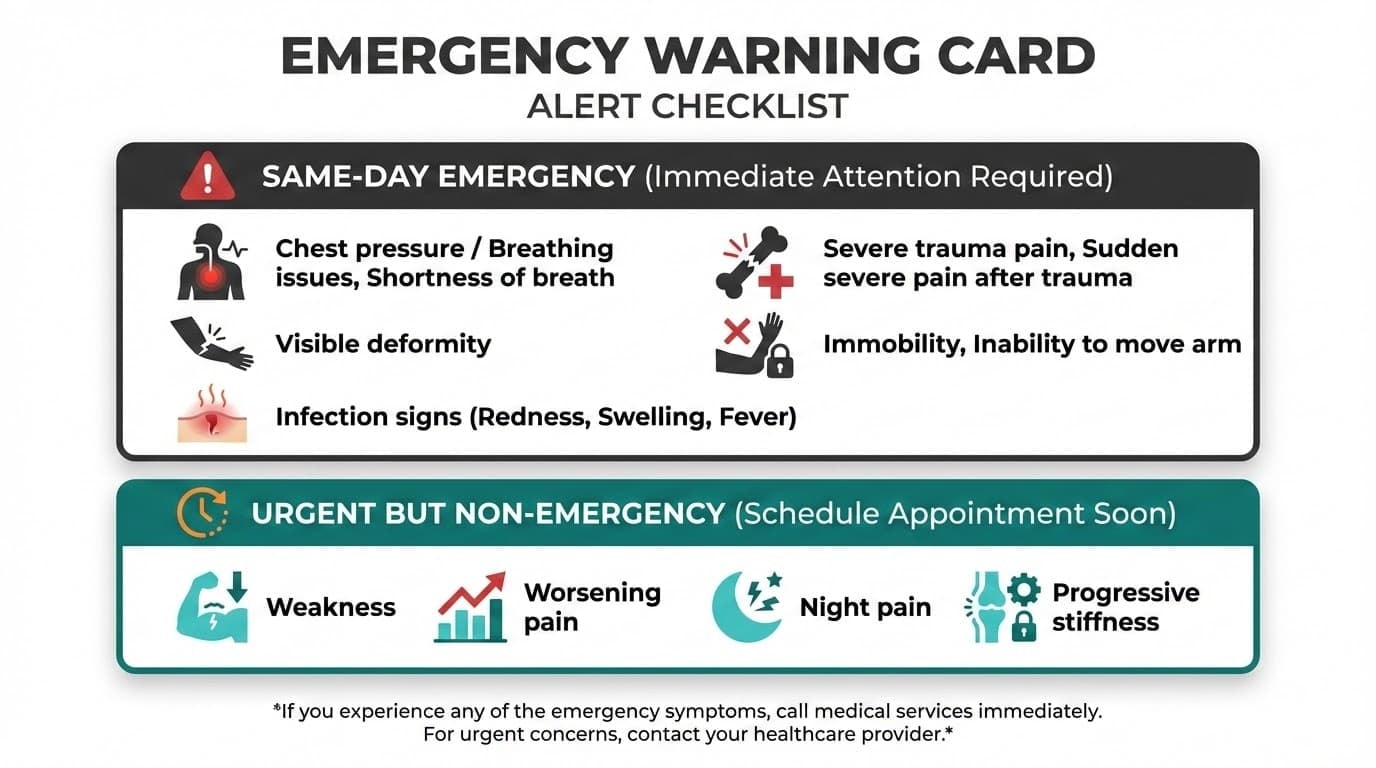
Most shoulder pain is not dangerous, but certain symptoms signal that something more serious may be happening. Knowing when to act quickly can protect your health and, in some cases, your life.
Same-Day Emergencies
Seek emergency care immediately if shoulder pain occurs with any of the following:
-
Chest pressure, shortness of breath, sweating, nausea, or pain spreading to the jaw or arm
-
Sudden severe shoulder pain after a fall, collision, or accident
-
Visible deformity of the shoulder or arm
-
Inability to move the arm at all after injury
-
Rapidly increasing redness, warmth, swelling, or fever around the shoulder
These signs can point to conditions such as a heart attack, fracture, unreduced dislocation, or joint infection, all of which require urgent treatment.
Urgent but Non-Emergency Concerns
Prompt medical evaluation within days is recommended if you notice:
-
Sudden weakness when lifting the arm after an injury
-
Shoulder pain that keeps worsening instead of improving
-
Severe night pain that prevents sleep for several nights in a row
-
Progressive stiffness with loss of movement
-
Pain returns quickly every time you resume normal activity
These symptoms may suggest acute rotator cuff tears, unstable joints, or inflammatory processes that benefit from early intervention.
Inflammatory or Rheumatologic Warning Signs
Some systemic conditions can present first as shoulder pain. Seek assessment if you experience:
-
New shoulder and hip pain with marked morning stiffness in adults over 50
-
Multiple joints are becoming swollen and painful over weeks
-
Fatigue, fever, or unexplained weight loss, along with shoulder pain
If you are ever unsure whether your symptoms are serious, it is safer to seek medical advice sooner rather than later.
How Clinicians Diagnose Shoulder Pain

Once urgent problems are ruled out, clinicians focus on identifying the true source of shoulder pain. This process relies more on careful reasoning than on any single test.
The Clinical History
Your provider will usually start by asking:
-
When and how the pain started
-
Whether there was a specific injury or a gradual onset
-
Which movements worsen or ease the pain
-
Whether pain disrupts sleep or daily tasks
-
Any prior shoulder injuries or surgeries
-
Relevant health conditions such as diabetes or thyroid disease
These details often narrow the diagnosis significantly before any exam begins.
The Physical Examination
A shoulder exam typically includes:
-
Active range of motion to see what you can move yourself
-
Passive range of motion to assess stiffness versus weakness
-
Strength testing of the rotator cuff and shoulder blade muscles
-
Special tests to check for impingement, instability, or labral injury
-
A brief neck exam to rule out nerve-related causes
The difference between active and passive movement is especially important in distinguishing conditions like frozen shoulder from rotator cuff pain.
The Role of Imaging
Imaging is used thoughtfully, not automatically:
-
X-rays help identify fractures, arthritis, or calcific deposits
-
Ultrasound can assess rotator cuff tendons dynamically
-
MRI is reserved for unclear cases or when surgery is being considered
Many people without shoulder pain have MRI abnormalities, so imaging findings alone do not equal a diagnosis.
Why Imaging Isn’t Always Needed
Most shoulder conditions are diagnosed accurately through history and examination alone. Imaging is most helpful when results will change treatment decisions, not simply to confirm that pain exists.
This approach avoids unnecessary testing, anxiety, and treatments that may not help.
What You Can Do: Self-Care, Treatment Options, and Next Steps

If you're dealing with shoulder pain, the first step is knowing there are real, evidence-backed ways to recover. Treatment usually starts conservatively and builds based on your symptoms and progress. Here’s what that can look like.
Self-Care at Home
In the early stages, easing pain and protecting your shoulder from further strain is key. Cold packs can help reduce inflammation and discomfort. Apply for 10 to 15 minutes at a time, especially after activity. Avoid heavy lifting or overhead movements, but try not to fully immobilize the shoulder unless your clinician advises it. Staying gently active helps prevent stiffness, especially in conditions like frozen shoulder.
Over-the-counter NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) can mitigate acute inflammation. For most mild shoulder pain, a mix of short-term rest and strategic movement goes a long way.
Physical Therapy and Exercises
For most causes of shoulder pain, whether rotator cuff related, frozen shoulder, or post-injury, structured physiotherapy is the foundation of recovery. Your program may begin with gentle mobility work, then progress to strengthening exercises targeting the rotator cuff and shoulder blade muscles.
A good therapist will also address posture, workspace setup, and any compensations that might be prolonging your symptoms. Progress takes time, but research shows that six to twelve weeks of consistent physical therapy leads to significant improvement for most people.
Alongside therapy and targeted exercises, many patients use shoulder braces to reduce daily strain. The Anaconda Brace is trusted by clinicians to support healing movement without full immobilization. It helps you stay active while protecting sensitive tissue.
Medications and Injections
Medication can support your recovery, but it is rarely the full solution. NSAIDs can provide short-term relief when pain flares.
In some cases, corticosteroid injections are used to control inflammation, especially for frozen shoulder or bursitis. However, repeated injections may weaken tendons over time, so they are best used sparingly and in conjunction with rehab.
Advanced Options Like PRP or Surgery
If pain persists despite months of guided rehab, your provider might recommend more advanced options. Platelet-rich plasma (PRP) injections show promise in some tendon injuries, helping to reduce pain and promote healing. Surgery is generally reserved for severe or non-responsive cases, such as large rotator cuff tears, instability, or advanced arthritis.
Recovery from surgery requires time and commitment to rehab, but it can restore function and reduce long-term pain when other options have not worked.
How Can Daily Habits Accelerate Shoulder Recovery?
Simple daily habits can speed up shoulder recovery, while knowing when to seek medical advice helps prevent setbacks
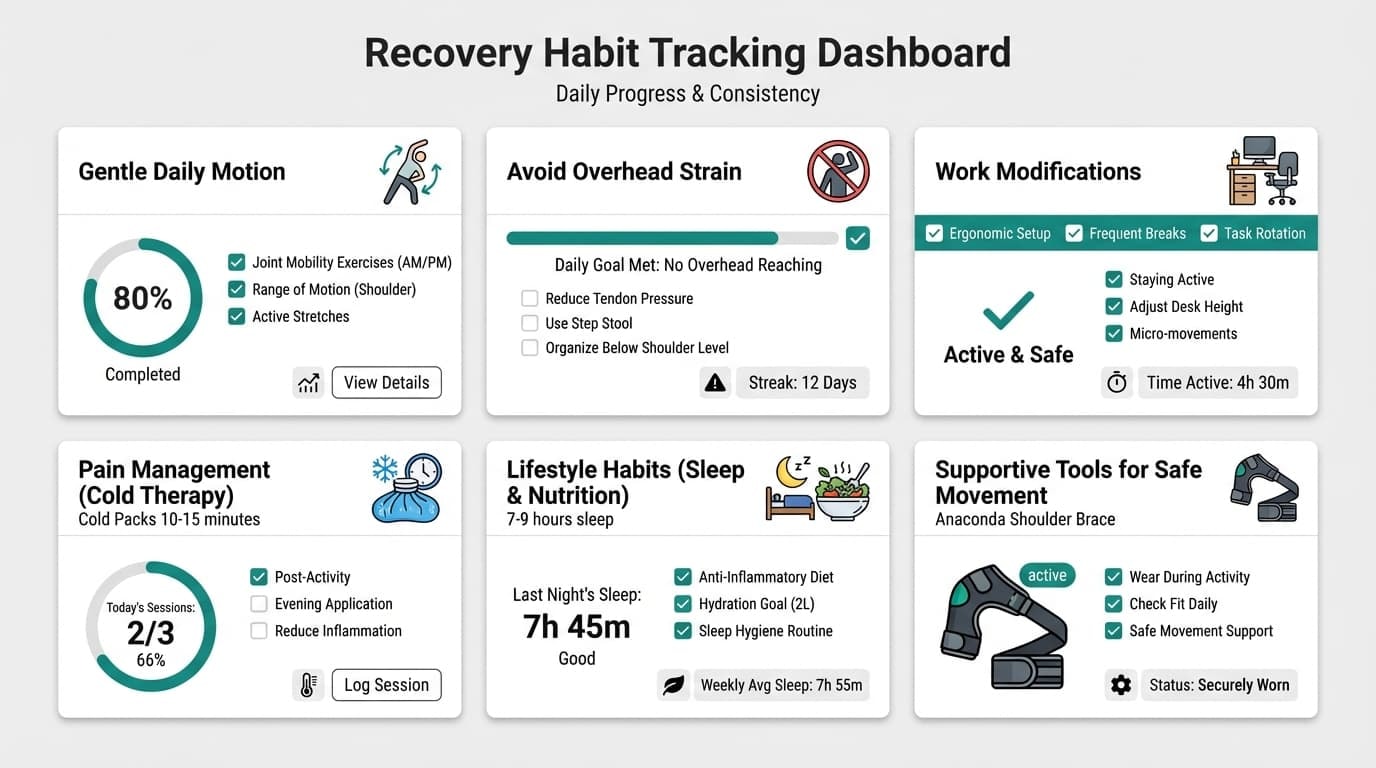
Use this illustration as a quick guide.
When to See a Doctor (Non-Emergency Cases)
Not all shoulder pain requires immediate care, but certain patterns suggest it’s time to get a professional evaluation. If your symptoms aren’t improving or are starting to interfere with daily life, seeing a healthcare provider can help you avoid long-term issues.
You should consider booking an appointment if:
-
Pain lasts longer than 4 to 6 weeks, even with rest and basic self-care.
-
You experience recurrent flare-ups that keep returning once you resume normal activities.
-
There's progressive stiffness or weakness, especially if your range of motion is shrinking or daily tasks are becoming harder.
Preparing for your visit can make it more effective. Take note of when the pain started, what makes it better or worse, how it affects your sleep and function, and any past injuries or treatments. The more context you provide, the more accurate and helpful the treatment plan can be.
Final Thoughts
Shoulder pain can be frustrating, but understanding the root cause is the first step toward recovery. Most cases improve with time, activity adjustments, and the right treatment approach, whether that’s home care, physical therapy, or medical support.
Staying gently active, protecting your shoulder during daily tasks, and getting help when pain lingers are all part of a smart recovery plan. For many people, using a supportive tool like the Anaconda Shoulder Brace can ease strain during healing while allowing safe movement.
If your pain is not improving, do not wait. The sooner you understand what is going on, the sooner you can get back to doing what you love, comfortably and confidently.
FAQs About Shoulder Pain
Quick answers to common concerns about causes, recovery, and when to get help.
Can shoulder pain go away on its own, or will I always need treatment?
In many cases, especially mild shoulder pain from overuse or rotator cuff tendonitis, shoulder pain can go away on its own. With rest, gentle movement, and ways to reduce inflammation, symptoms often improve within a few weeks. However, shoulder injuries like rotator cuff tears, frozen shoulder, or shoulder arthritis usually need physical therapy or personalized treatment plans. If shoulder pain keeps returning or limits daily use, professional care helps prevent long-term problems.
How can I tell if my shoulder pain is coming from my neck instead?
Shoulder pain originating in the neck often travels past the shoulder and down the arm, a phenomenon called referred pain. You may experience pain with tingling or numbness, and symptoms often change with neck movement rather than shoulder movement. Pain from the shoulder joint or glenohumeral joint is usually worse with lifting or rotating the arm. Because overlap is common, a physical therapist often checks both areas.
Is it safe to keep exercising or playing sports with shoulder pain?
Playing sports with shoulder pain can be safe if discomfort is mild and settles within hours. Sharp pain, sudden weakness, or worsening pain over time are signs to stop. Gentle motion exercises help keep shoulder muscles flexible, but heavy overhead training can worsen rotator cuff injuries. If pain started after trauma or persists, physical therapy guidance is recommended.
Do I need an MRI for shoulder pain right away?
You usually do not need imaging tests like an MRI right away for shoulder pain causes. Many problems, such as rotator cuff tendonitis, fluid-filled sac irritation, or acromioclavicular joint pain, are diagnosed with an exam. Imaging tests are used when shoulder fractures, full rotator cuff tears, or labral injuries are suspected. Your clinician decides based on symptoms and exam findings.
How long does it usually take to recover from common shoulder problems?
Recovery time depends on the cause of shoulder pain and its severity. Minor overuse pain often improves in 2 to 6 weeks, while rotator cuff injuries may take months with physical therapy. Adhesive capsulitis, or frozen shoulder, can last 1 to 3 years, especially in the early stages when pain is severe. Shoulder arthritis and post injury recovery vary widely and benefit from individualized care plans.














