Shoulder replacement surgery is initially painful, with discomfort peaking during the first 48 to 72 hours.
However, clinical data from 2025 indicates that average pain levels drop to 1.8/10 by the three-month mark, representing an 89.1% recovery rate for anatomic replacements.
This trajectory is significantly more favorable than chronic pre-operative arthritis pain, which typically averages 6–7/10.
The challenge is that this pain is rarely straightforward.
Neck and shoulder pain often manifests at the base of the cervical spine, radiating into the acromion or scapular region during active movement. That overlap makes it hard to tell whether the issue is muscular, joint-related, or nerve-driven, and easy to second-guess the next step.
We see this pattern every day. Athletes and active people come to us with the same questions. What is causing the pain? What actually helps. And when should they be concerned? The good news is that most neck and shoulder pain responds well to simple, evidence-based strategies when applied early and consistently.
This guide analyzes the biological and mechanical recovery trajectory of shoulder arthroplasty, specifically addressing:
-
What is the standard post-operative pain timeline?
-
How do anatomic and reverse procedures differ in pain outcomes?
-
Which multimodal management protocols are most effective in 2026?
Key Takeaways
-
Most neck and shoulder pain is nonspecific and not caused by serious disease. Dangerous underlying causes like cancer, infection, or vascular injury account for less than 1% of cases, but recognizing red-flag symptoms remains essential.
-
Staying active, using heat, and doing simple evidence-based exercises work better long-term than rest, collars, or slings for most nonspecific pain.
-
Routine imaging (X-rays, MRI, CT) is usually unnecessary in the first 4–6 weeks unless you’ve had major trauma, worsening neurologic signs, or other red flags.
-
For rotator cuff–related shoulder pain, targeted exercise and physical therapy are at least as effective as steroid injections in the medium- and long-term.
-
Start today: apply heat for 15–20 minutes, take posture breaks every hour, and try 2–3 gentle neck or shoulder exercises.
How Common Are Neck and Shoulder Problems?
Neck and shoulder pain is extremely common. We see neck and shoulder discomfort in people of all ages and activity levels. Shoulder and neck pain affects athletes, desk workers, and anyone who spends long hours sitting, lifting, or repeating the same movements.
To give you a sense of scale:
-
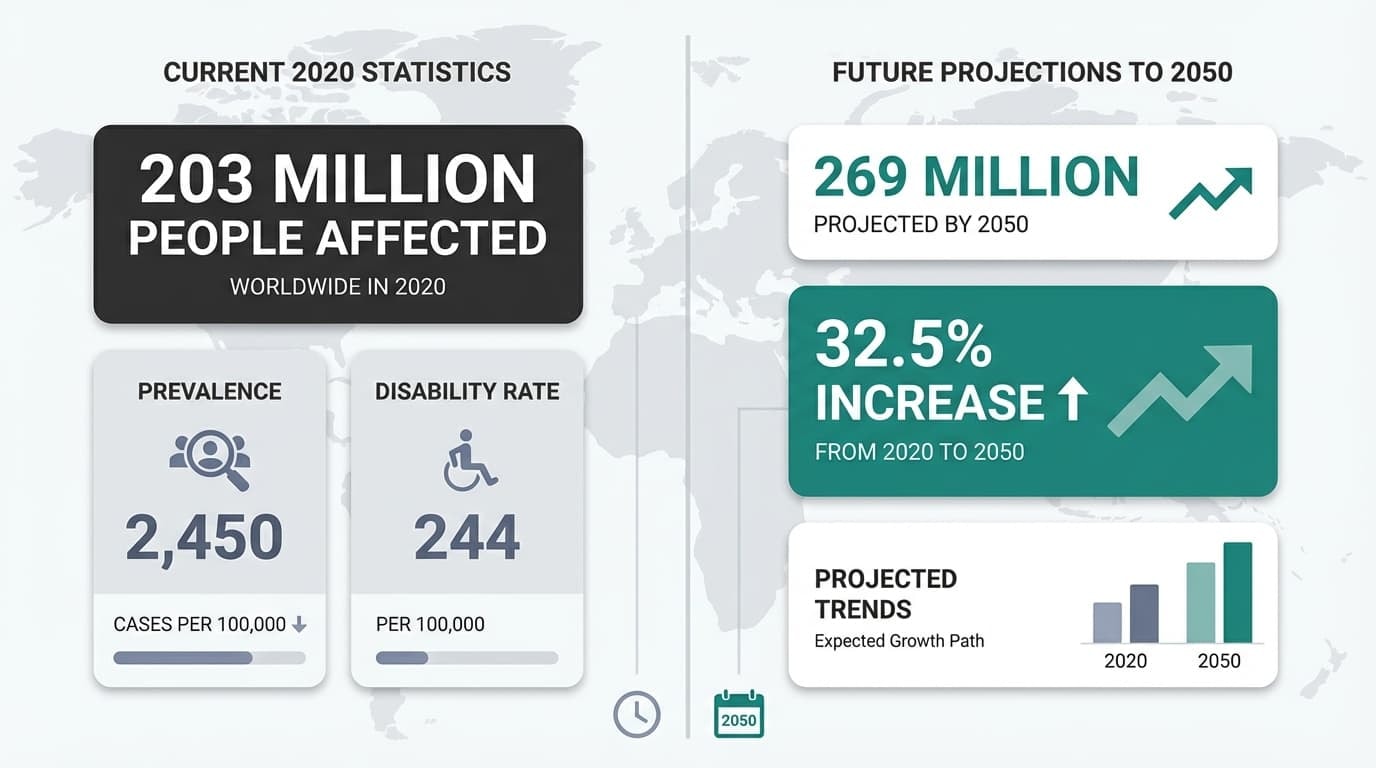
In 2020, about 203 million people worldwide were affected by neck pain
-
Much of this pain involves the cervical spine, surrounding neck muscles, and the structures connecting the neck and shoulder
-
The global prevalence reached 2,450 cases per 100,000 people, with a years lived with disability rate of 244 per 100,000
This means neck and shoulder pain is not just common; it often lasts long enough to affect daily comfort and movement.
The numbers are still going up. According to the same research, by 2050, estimates suggest 269 million people globally will experience neck and shoulder pain. That is a 32.5% increase from 2020, largely due to population growth and aging.
Shoulder pain on its own is also among the most common musculoskeletal complaints. Many cases involve the shoulder’s ball and socket joint, including rotator cuff injuries, rotator cuff tears, or frozen shoulder. It is also common for shoulder pain and neck symptoms to overlap, which adds to how widespread this issue feels.
Neck and Shoulder Anatomy in Everyday Terms
When people experience neck and shoulder pain, they often assume there must be a single clear structure at fault. In reality, the neck and shoulder function as a connected system.
Understanding that connection helps explain why pain can feel confusing without meaning that something is seriously wrong.
The Cervical Spine
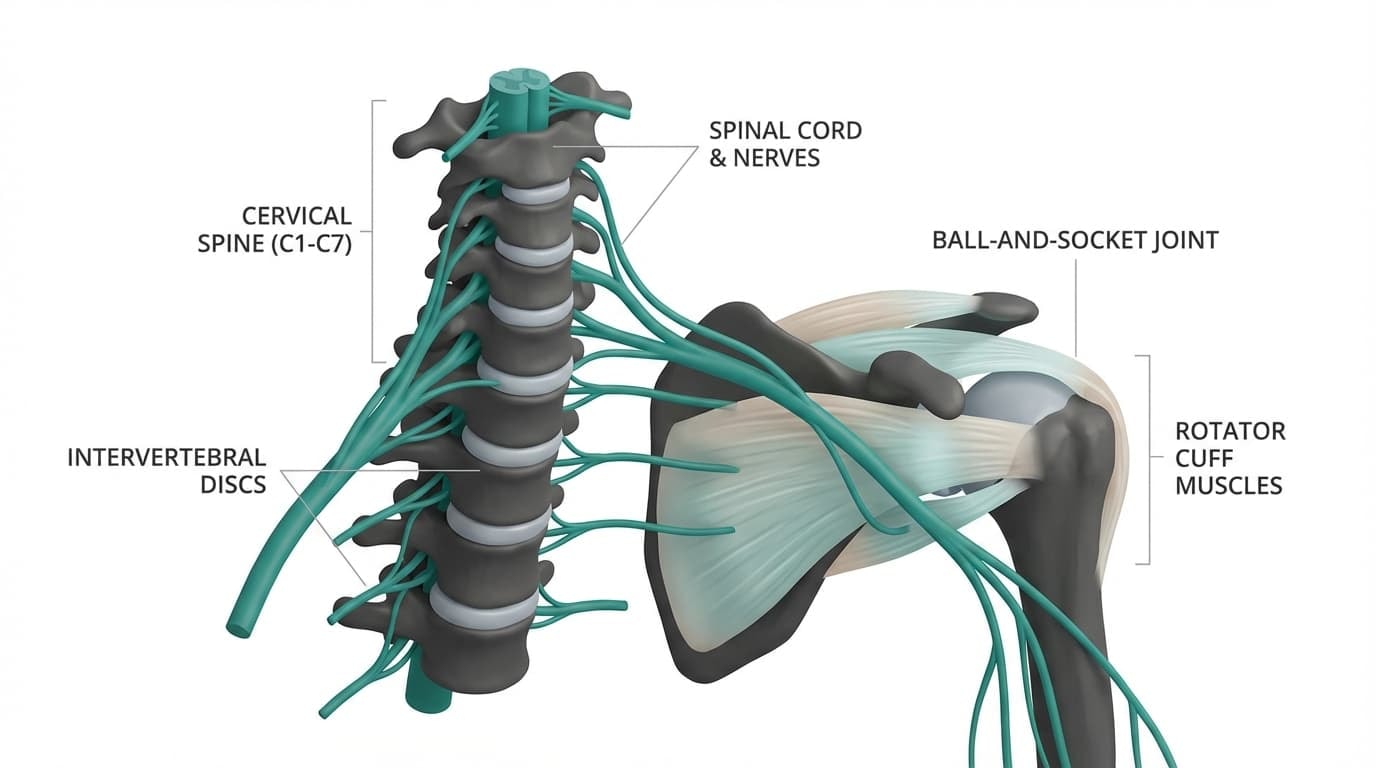
The cervical spine consists of seven vertebrae (C1–C7) and serves as the primary support for the head's weight.
According to 2025 German S3 Guidelines, most discomfort in this region is 'nonspecific,' meaning symptoms lack a single identifiable structural pathology in the majority of cas
Running through the center is the spinal cord, with nerves branching out toward the shoulders and arms.
The surrounding neck muscles support the weight of your head and control motion throughout the day. According to a 2025 German S3 guideline, most neck pain is defined anatomically and classified by duration rather than by a specific structural cause. When no clear structural issue is found, it is labeled nonspecific, which applies to the majority of cases.
This explains why discomfort can show up even without obvious damage from a neck injury.
The Shoulder Joint
The shoulder joint is a ball-and-socket structure. The top of the arm bone sits in a shallow socket on the shoulder blade, allowing a wide range of motion. That mobility is useful, but it also means the shoulder relies heavily on muscle coordination for stability.
The rotator cuff plays a central role here. These muscles help guide the joint during movement and are commonly involved in rotator cuff injuries and other shoulder injuries. Supporting structures like ligaments and the labrum help stabilize the shoulder, but the shoulder is designed to move freely rather than lock into place.
Why Pain Can Travel
Neck and shoulder structures share nerves and muscles. Because of this overlap, irritation in one area can be felt somewhere else, sometimes as arm pain or tension around the left shoulder.
Large guideline reviews, including a 2024 analysis of international neck pain guidelines, show that potentially dangerous underlying causes account for less than 1% of cases. Most pain reflects how these connected structures respond to load and movement, not damage or disease.
Understanding the anatomy helps explain why pain can shift and why location alone does not always tell the full story.
Common Causes of Neck and Shoulder Pain
Once you understand how closely the neck and shoulder are connected, the causes of pain start to make more sense. Most discomfort in this area does not come from a single injury. It develops when certain tissues are asked to do more than they can comfortably handle.
Where Neck Pain Often Starts
Neck pain usually builds from a few common patterns rather than a single moment or injury. The most frequent sources include:
-
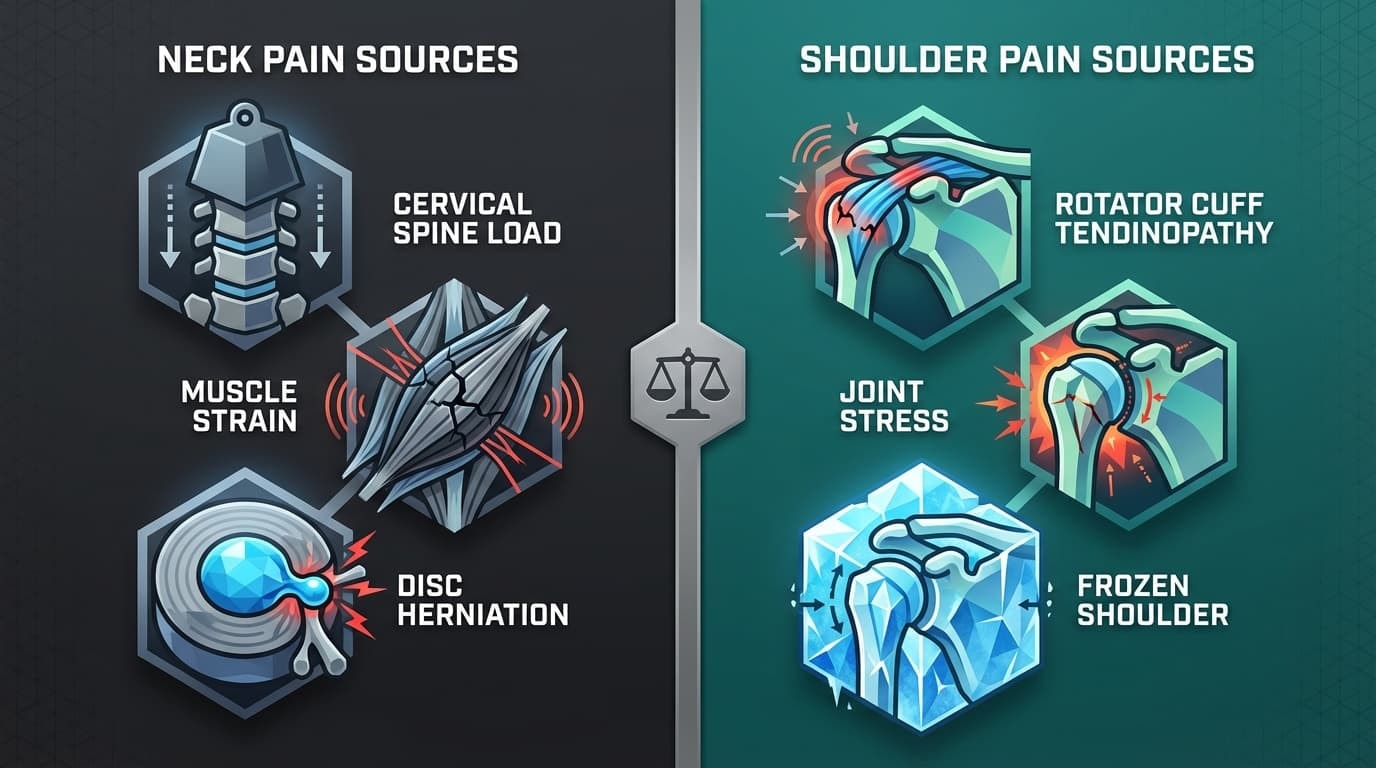
Ongoing load on the cervical spine and surrounding neck muscles, especially from poor posture, such as long periods with the head positioned forward
-
Muscle strain caused by sudden movements, awkward sleeping positions, or repeated tasks that overload muscles faster than they can recover
-
Age-related changes in the cervical spine, known as cervical spondylosis, often appear on scans even in people without symptoms
-
Disc changes or a disc herniation can irritate nearby nerves and contribute to pain that travels beyond the neck and into the arm
Where Shoulder Pain Often Starts
When pain comes from the shoulder itself, it usually relates to how the joint and its supporting tissues handle repeated movement and loading. Common sources include:
-
Stress on the structures that control the movement of the shoulder joint, which relies on muscle coordination rather than stiffness for stability
-
Overuse or repeated loading of the rotator cuff, leading to rotator cuff tendinopathy
-
Larger or long-term overload that contributes to rotator cuff tears, which may or may not cause immediate symptoms
-
Gradual stiffening from frozen shoulder, or joint surface wear from shoulder osteoarthritis, both of which can limit movement over time
The Role of Lifestyle and the Nervous System
Structure is only part of the picture. Stress, poor sleep, and sustained muscle tension can intensify neck and shoulder pain. Clinical guidelines consistently note that pain reflects both tissue load and the nervous system's response to that load. This is why pain intensity does not always match what appears on imaging.
Is the Pain Coming From My Neck or My Shoulder?
Because the neck and shoulder share nerves and muscles, pain does not always stay neatly confined to one area. This is why careful assessment matters more than guessing based on location alone.
Signs Pain May Be Coming From the Neck
When the neck is the primary source, pain often behaves in a more spreading or position-dependent way. Common signs include:
-
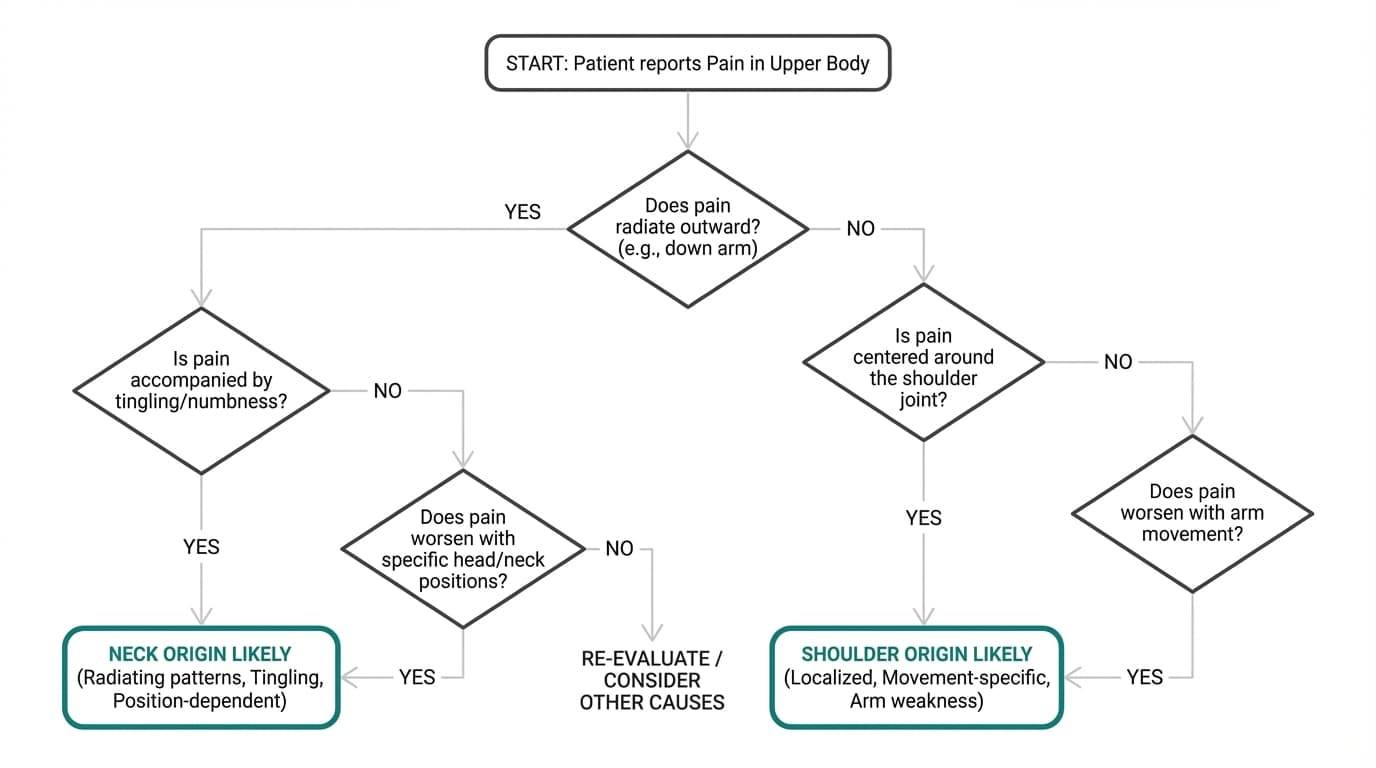
Pain that starts in the neck and radiates outward into the shoulder or down the arm
-
Arm pain accompanied by tingling, numbness, or altered sensation
-
Symptoms that change with neck movement, head position, or holding the neck in one posture for too long
Signs Pain May Be Coming From the Shoulder
When the shoulder itself is involved, pain tends to stay more localized and movement-specific. Typical signs include:
-
Pain centered around the shoulder rather than the neck
-
Discomfort that worsens with specific arm movements, especially reaching overhead or away from the body
-
Weakness or pain during certain shoulder movements without clear involvement of neck motion
A Helpful Way to Think About It
Neck-related pain often refers outward and feels less precise. Shoulder joint pain is usually more focused and tied to how the arm moves. This distinction does not replace professional evaluation, but it helps explain why neck and shoulder pain can feel so hard to pinpoint.
Guidelines emphasize that understanding these patterns is part of careful clinical assessment and helps avoid jumping to conclusions too early.
When Neck or Shoulder Pain Needs Urgent Care
Most neck and shoulder pain is not dangerous. But there are specific situations where pain should not be ignored or monitored at home. Knowing these red flags helps you act quickly and confidently when it matters.
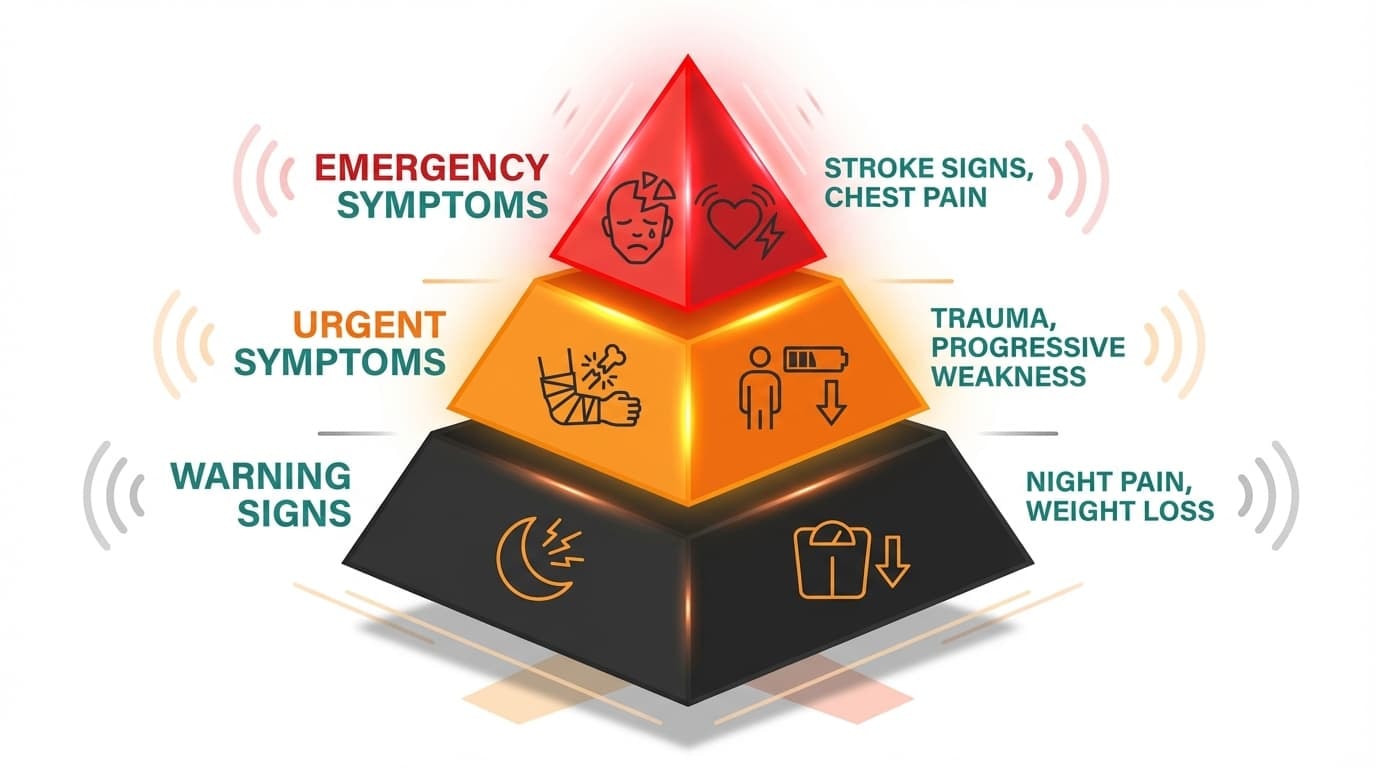
Emergency Symptoms
Seek immediate medical attention if neck or shoulder pain is accompanied by any of the following:
-
Stroke-like signs such as sudden confusion, trouble speaking, facial drooping, or weakness on one side of the body
-
Chest pain combined with pain in the left shoulder, jaw, or arm, especially if it occurs with shortness of breath, nausea, or sweating
-
Loss of bladder or bowel control alongside neck pain, which may signal pressure on the spinal cord
These symptoms require urgent evaluation and should not be pushed through or self-managed.
When to Seek Urgent Medical Evaluation
Some symptoms are not emergencies but still need timely medical care:
-
Neck or shoulder pain after significant trauma, such as a fall or car accident
-
Progressive weakness, loss of coordination, or increasing numbness
-
Fever, unexplained weight loss, or a known history of cancer, combined with new neck or shoulder pain
Pain that spreads across the shoulder blade, steadily worsens, or is paired with systemic symptoms should be assessed by a healthcare professional.
Systemic Warning Signs
Arrange a medical review if you notice:
-
Night pain that consistently wakes you from sleep
-
Ongoing, unexplained weight loss
-
Pain that continues to worsen over time rather than stabilizing or improving
These patterns suggest the need for evaluation rather than continued self-monitoring.
Do I Need an X-ray, MRI, or Scan?
It is very common to wonder whether imaging is needed when pain does not resolve right away. In most cases, scans are not the first or most useful step.
Why Imaging Is Usually Not Needed Early
For new or recurring neck and shoulder pain without red flags, guidelines recommend starting with a careful history and physical exam. This clinical assessment often provides more meaningful information than early imaging.
Scans frequently show age-related findings, such as bone spurs or joint and soft-tissue wear. These changes are common even in people without pain and do not always explain symptoms. Seeing them too early can increase worry without improving care decisions.
When Imaging Is Appropriate
MRI or CT imaging may be considered when:
-
Symptoms are severe, progressive, or not improving after several weeks
-
There are signs of nerve involvement or possible spinal cord compression
-
A significant injury raises concern for structural damage
For shoulder injuries, imaging may be useful when symptoms suggest a serious soft tissue injury or when planning further care.
Evidence-Based Treatment for Neck Pain
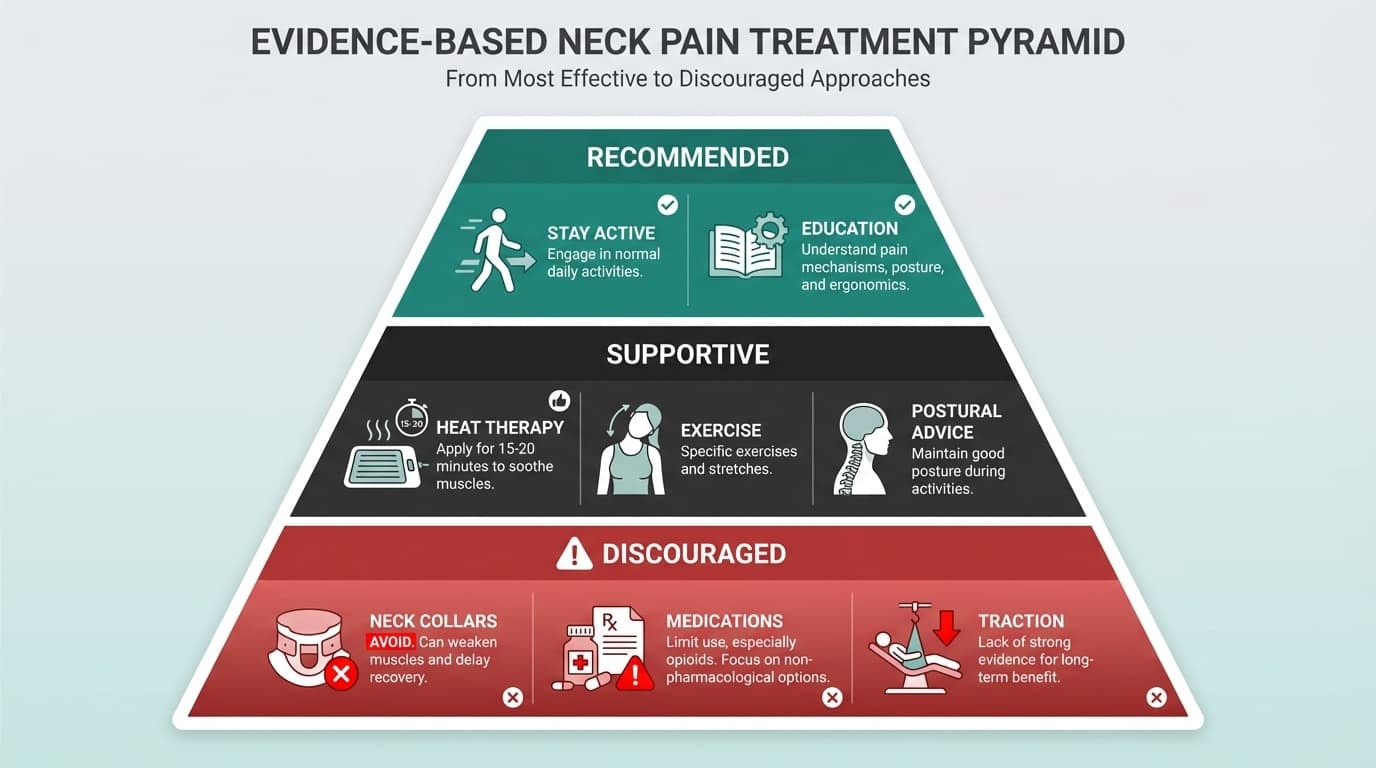
Once serious causes are ruled out, the goal is not to shut movement down. It is to keep you moving in a way your neck can tolerate and gradually handle more of again. That approach is backed strongly by evidence. Guidelines consistently show that activation-focused care produces large improvements in pain and function, with effect sizes exceeding those of most passive treatments.
Stay Active and Rebuild Tolerance
Neck pain responds best when movement is reintroduced early and progressed gradually. Complete rest often makes symptoms linger longer.
This usually means:
-
Gentle daily movement instead of avoiding motion
-
Pacing activity and gradually increasing tolerance
-
Avoiding long periods of stillness or bed rest
-
Returning to normal daily tasks as symptoms allow
The goal is not to push through pain, but to stop guarding the neck unnecessarily and allow normal motion to return.
Education Is Part of Treatment
Understanding what neck pain represents changes how the body responds to it. Learning how nerves and muscles recover, and why pain does not always signal damage, helps reduce fear and hesitation around movement.
Clinical guidelines show that patient education produces meaningful reductions in pain and fear of movement. When people feel more confident in what they are experiencing, they tend to move more freely and recover more consistently.
Heat and Cold Can Support Comfort
Simple physical modalities can help manage symptoms while staying active.
-
Heat, such as warm packs or showers, used for 15 to 20 minutes, is strongly supported and commonly helpful for muscle tension
-
Cold can be used early after a strain if it feels soothing
-
When used sensibly, both options carry minimal risk
These tools are about comfort, not correction.
Medications Have Limits
Over-the-counter anti-inflammatory medications may provide short-term relief for some people, but the average benefit is modest. Research shows pain reductions are often small and temporary.
Long-term or frequent use increases the risk of stomach irritation, ulcers, and cardiovascular side effects. For this reason, medications should be used sparingly and only as support, not as a substitute for movement and recovery.
What Guidelines Advise Against
Some approaches are consistently discouraged because they delay recovery or increase risk without improving outcomes.
These include:
-
Prolonged use of neck collars or immobilization
-
Muscle relaxers are limited in their benefit and have side effects
-
Opioids are high-risk and low-effectiveness
-
Mechanical traction and electrotherapy, which lack meaningful evidence
-
Kinesiotaping, when used alone, can promote passivity
Shutting the neck down tends to prolong the problem rather than solve it.
Optional Adjuncts
Hands-on treatments such as manual therapy, mobilization, massage, or acupuncture can be used selectively, particularly for persistent symptoms. When they are helpful, they work best as add-ons that support active recovery rather than replace it.
The consistent message across guidelines is clear. Neck pain improves when movement is restored, confidence is rebuilt, and passive approaches stay in a supporting role.
Evidence-Based Treatment for Rotator Cuff–Related Shoulder Pain
When shoulder pain comes from the rotator cuff, the evidence is very clear. Exercise-based care is most effective for most cases, including tendinopathy, partial tears, and common shoulder overuse injuries.
The shoulder is built for movement. As the rotator cuff and surrounding soft tissues gradually relearn how to handle load, pain, and function, painand function tend to improve together.
What the Evidence Tells Us
Well-designed rehab programs focus on controlled movement, strength, and coordination between the shoulder and the scapula. Over time, this restores stability and reduces symptoms like arm pain or weakness during lifting and reaching.
Large research reviews consistently show that these structured programs outperform generic or passive approaches, especially for improving function.
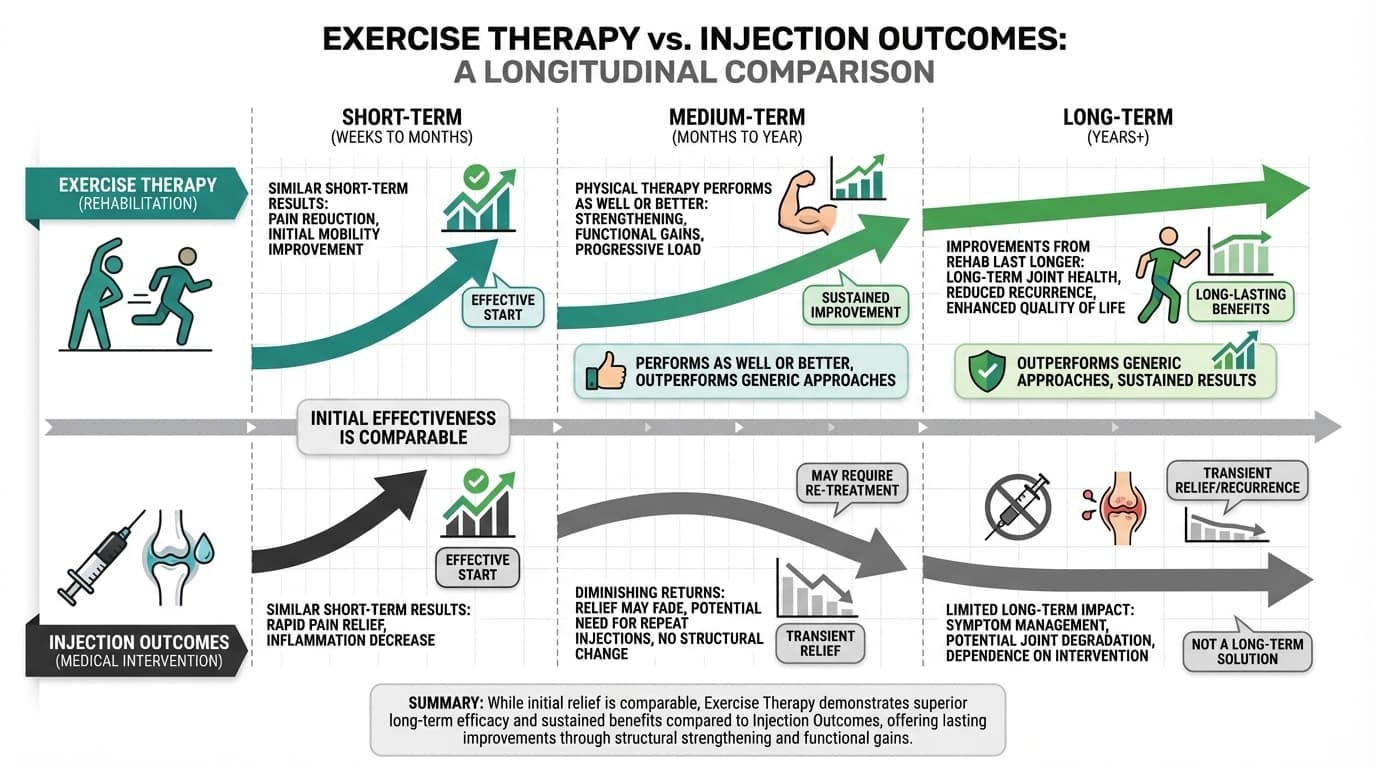
Exercise vs Injections
Injections can reduce pain in the short term, but they do not rebuild rotator cuff strength or tolerance.
When compared directly:
-
Short-term results are often similar
-
Over the medium and long term, physical therapy performs as well or better than
-
Improvements from rehab tend to last longer
This is why injections are usually considered supportive, not the main solution, unless severe pain is limiting progress.
When Surgery Comes Into the Picture
Surgery is not the first step for most shoulder injuries. It is typically considered when there is:
-
A full-thickness tear with clear strength loss
-
Persistent symptoms after months of proper rehab
-
Structural damage that cannot recover with loading
Many people improve without surgery, even when scans show changes like bone spurs or tendon tears.
Why Guidance Matters
A physical therapist helps tailor loading to your shoulder, accounting for how it works with nearby structures, such as the trapezius and neck muscles. This matters because shoulder pain is often influenced by movement patterns, tense muscles, and even prior neck injury, not just the shoulder itself.
Home Strategies You Can Start Today
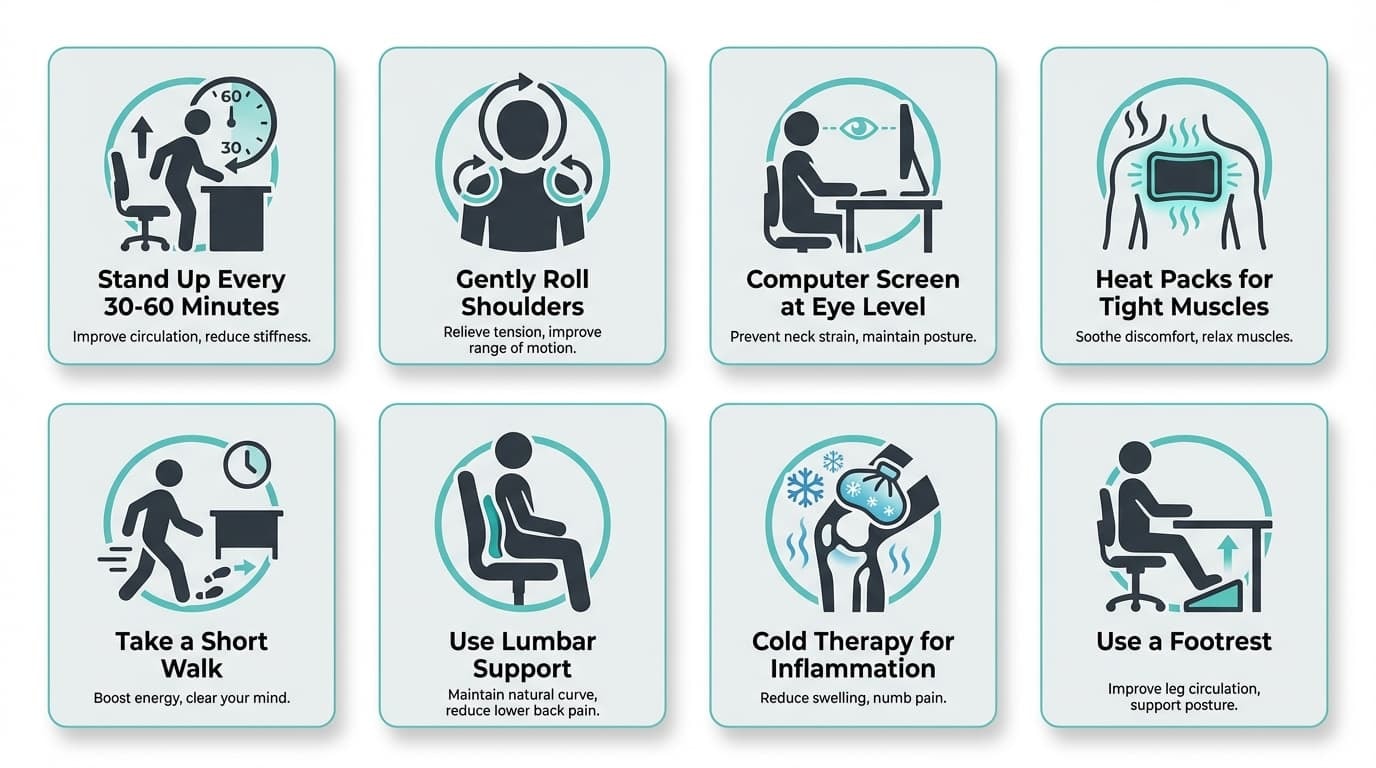
If your symptoms are nonspecific and do not require immediate medical attention, day-to-day habits often shape how quickly the body settles.
Relief rarely comes from doing more. It usually comes from doing small things consistently.
Keep the Body Moving
Long periods of sitting or inactivity can cause muscles and nerves around the neck and shoulders to stiffen. Simple resets help:
-
Stand up every 30–60 minutes
-
Gently roll the shoulders
-
Turn the head side to side
These brief movements reduce discomfort without forcing the body.
Use Heat or Cold for Comfort
Heat and cold can help you stay comfortable while you stay active. Warm showers or heat packs often help tight muscles relax and provide short-term relief. Cold can soothe irritation and help reduce inflammation. Let comfort guide the choice.
Let Posture Change
Posture does not need to be perfect. It needs to change. Keep your computer screen near eye level, let your shoulders drop away from your ears, and avoid long static positions. Variety matters more than rigid posture rules.
When Extra Support Helps
Support tools can be useful when discomfort or instability makes movement feel uncertain. The Anaconda Shoulder Brace provides targeted 3D compression that supports the shoulder joint without locking it down. It stays in place during daily activity and training, helping reduce unnecessary movement while allowing natural motion. Many athletes use it to stay active and confident while rebuilding tolerance.
Manage Tension, Not Just Pain
Stress influences how symptoms feel. Psychological stress increases muscle tone and alters how the nervous system interprets signals from the body. Short breathing pauses during the day can help reset tension and make neck and shoulder discomfort easier to manage.
Safe Exercises for Neck and Shoulder Pain
When pain has been lingering, it’s normal to feel cautious about movement. These exercises are not about pushing through discomfort or “fixing” your body. They are meant to help you move again with confidence, at a pace your body can tolerate.
If pain becomes sharp, spreads down the arm, or causes new numbness, pause and reassess. Listening to those signals matters.
Start With Gentle, Familiar Motion
For the neck, simple movements like chin tucks, side bending, and slow rotation help reintroduce motion without irritating sensitive tissues. For the shoulder, pendulum swings, wall-assisted arm lifts, and light shoulder blade squeezes help coordinate the shoulder joint with the surrounding muscles.
These movements may feel almost too easy at first. That is intentional. Early comfort builds trust in movement, which supports longer-term progress.
Let Comfort Guide Progress
Stay within a pain-free range, breathe normally, and allow progress to unfold over days or weeks rather than sessions. Consistency matters more than intensity.
This approach is the same one used by clinicians and coaches who work with active people every day. It’s also how many athletes supported by Anaconda rebuild tolerance safely, without rushing or unnecessary setbacks.
If symptoms persist or feel unclear, a professional can help fine-tune direction and volume to keep movement safe and effective.
Medications, Injections, and Surgery
Medications, injections, and surgery are tools, not starting points.
Short-term pain medications may help during flares, but they do not correct the movement or load patterns contributing to symptoms. Long-term use carries risks and should be limited.
Injections can offer temporary relief, particularly when irritated tendons or soft tissues are involved, but research shows they do not consistently outperform movement-based care over time.
Surgery is usually reserved for clearly defined structural problems or persistent symptoms that do not improve with conservative care. This is where the right diagnosis matters most.
What to Avoid With Neck and Shoulder Pain
Some approaches feel productive in the moment, but often slow progress rather than support it.
Long stretches of immobilization, relying only on passive treatments, repeatedly chasing X-rays, or leaning on medication without movement tend to increase frustration rather than relief. Many imaging findings are common even in people without active injuries, and they do not always explain why pain is there or why it lingers.
Progress usually stalls when movement is avoided entirely or when care becomes reactive rather than consistent. The goal is not to ignore pain, nor to let it dictate every decision.
Living Well With Recurrent or Chronic Neck and Shoulder Pain
Ongoing neck or shoulder pain can affect work, sleep, and confidence, but it does not mean your body is broken or beyond recovery.
-
Pacing makes a difference. Breaking demanding tasks into smaller blocks, alternating activities, and avoiding the boom-and-bust cycle help the body rebuild tolerance steadily. Small, repeatable movement often outperforms extremes.
-
Mental load matters too. Chronic discomfort is shaped by the nervous system as much as the tissues themselves. Stress can amplify symptoms, while addressing it directly often makes pain easier to manage over time.
-
Your setup counts. Simple adjustments to chair height, screen position, and taking frequent breaks matter, especially during long workdays or driving-heavy routines.
When flare-ups happen, having a plan helps. Knowing when to ease back temporarily, when gentle movement or heat is enough, and when symptoms call for medical attention helps prevent setbacks from spiraling out of control.
This is also where supportive gear can fit into the bigger picture. Many athletes turn to tools like the Anaconda Shoulder Brace when shoulder discomfort or instability begins to interfere with training. It’s built to stay in place during movement, providing targeted support without locking the joint.
That philosophy reflects how Anaconda operates as a whole. More than 300,000 athletes train with Anaconda gear because it supports movement instead of restricting it, and the feedback comes from real training environments, not theory.
Final Words
Neck and shoulder pain is common, but it is rarely random. Most symptoms build over time from how the body handles load, posture, and recovery, especially during long periods of sitting, training, or screen use. Understanding the common causes, from stressed muscles and irritated tendons to sensitive nerves, helps you respond calmly instead of guessing or rushing into X-rays or scans that often do not change outcomes.
The goal is always the right diagnosis, knowing when self-care is enough and when medical attention matters, such as warning signs linked to serious issues like a heart attack. Most people can find relief by staying active, adjusting habits, and supporting recovery early.
For athletes managing shoulder discomfort, Anaconda fits naturally into that approach. Built to support movement without restriction, Anaconda gear is trusted by over 300,000 athletes to train confidently while rebuilding tolerance and protecting against further injuries.
FAQs
Use these quick answers to understand what to watch, what to do, and when to seek help.
How long should I wait before seeing a doctor about neck or shoulder pain?
You should wait about 1–2 weeks if neck or shoulder pain is mild, came on gradually, and improves with basic self-care. If pain is severe, disrupts sleep, limits daily activity, or does not improve after 2–4 weeks, medical evaluation is appropriate. Seek care sooner if pain follows trauma or worsens steadily. Sudden neurological or systemic symptoms always need immediate attention.
Can my neck and shoulder pain be caused by stress alone?
Stress alone usually does not cause structural damage, but it can significantly increase muscle tension and amplify pain signals. Ongoing stress and poor sleep are strongly linked to higher pain intensity and longer recovery times. Managing stress alongside movement and activity often reduces symptoms. This is a real and common contributor, not “all in your head.”
Is it safe to keep exercising if I have neck or shoulder pain?
In most cases, yes, it is safe and recommended to keep moving within comfortable limits. Resting too much often leads to increased stiffness and weakness. Avoid sharp or worsening pain, and modify movements rather than stopping altogether. A physical therapist can help adjust exercises safely if needed.
Will my neck or shoulder pain become chronic if I don’t get an MRI or injection?
Neck or shoulder pain does not become chronic because you skipped early imaging or injections. Recovery is more closely tied to activity, load management, and daily habits. Most people improve with active self-management and time. Scans and injections are tools for specific cases, not requirements for recovery.
Can I prevent neck and shoulder pain from coming back?
You can reduce flare-ups by maintaining regular movement, improving posture, and avoiding long periods in one position. Simple daily mobility and strength work builds resilience over time. Paying attention to early warning signs helps you respond before pain escalates. Consistency matters more than intensity.














