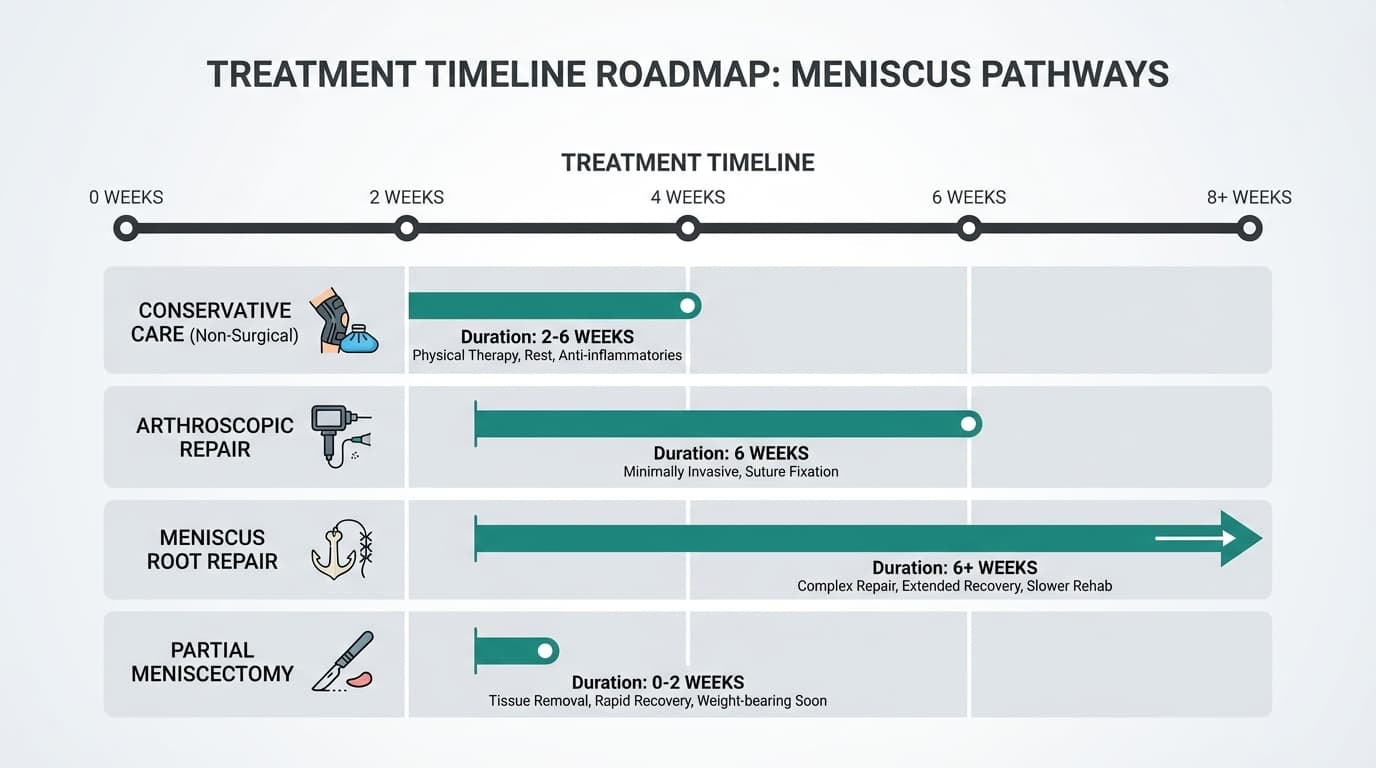
Most patients must wear a knee brace for 4 to 12 weeks following a meniscus tear. Conservative care typically requires 2–6 weeks of activity-specific bracing, while surgical repairs mandate a minimum of 6 weeks in a hinged brace to protect healing tissue and prevent re-tears during the critical collagen-formation phase.
This recovery guide analyzes the primary variables for brace duration:
-
How does the specific tear type (Radial vs. Root) change the timeline?
-
What is the 0–12 week phase-by-phase bracing protocol?
-
When is it safe to discontinue brace use during daily activities?
Ready to take the guesswork out of your recovery? Let’s get started.
Key Takeaways
-
Orthopedic protocols in 2026 mandate 4–12 weeks of bracing to stabilize the femoral-tibial joint, reducing meniscal shear stress by up to 60% during the initial inflammatory phase.
-
Root repairs and complex tears typically require the longest bracing, often 6+ weeks in full extension, then a gradual weaning period. In contrast, a partial meniscectomy may require little or no bracing at all.
-
Brace duration is personalized based on your tear type, whether surgery was performed, pain level, knee stability, and specific instructions from your surgeon and physical therapist.
-
Over-wearing a brace can cause stiffness and muscle loss, while removing it too early can increase re-tear risk, especially during the critical first 6 weeks when tissue is most vulnerable.
-
The sections below break down time frames by tear type, treatment plan, and daily-life situations, including walking, sleeping, work, and sport.
How Long Should You Wear a Knee Brace for a Torn Meniscus?
Most people wear a knee brace for 4 to 12 weeks, but the exact timeline depends on your tear type, treatment plan, and how your knee heals.
If your tear is small and stable and treated without surgery, you may only need the brace during painful activities for 2 to 4 weeks.
2025 Clinical guidelines from the American Academy of Orthopaedic Surgeons (AAOS) confirm that standard repairs require 4 to 6 weeks of bracing to ensure the integrity of the suture site against rotational forces.
More complex injuries, such as root tears or multidirectional tears, often need 6 or more weeks with the brace locked, followed by a gradual transition that can extend to 12 weeks total.
Typical timelines look like this:
-
Conservative care without surgery: brace during activity for 2 to 6 weeks, tapering as pain improves
-
Arthroscopic repair: about 6 weeks in a hinged brace, starting locked at 0 degrees and slowly unlocking
-
Meniscus root repair: at least 6 weeks of non-weight bearing with the brace locked for walking and often sleeping
-
Partial meniscectomy: no brace at all or 1 to 2 weeks for comfort only
These ranges reflect modern 2024 and 2025 orthopedic rehabilitation protocols. Your surgeon or physical therapist will adjust the schedule based on surgical findings, swelling, strength, and overall progress.
When discussing how long to wear a brace, both total weeks and daily wear time are considered. Early in recovery, the brace may be worn for nearly all of the day. As healing improves, use is often limited to higher-risk activities, such as outdoor walking, stairs, or more extended periods on your feet.
What Factors Influence the Duration of Knee Brace Use?
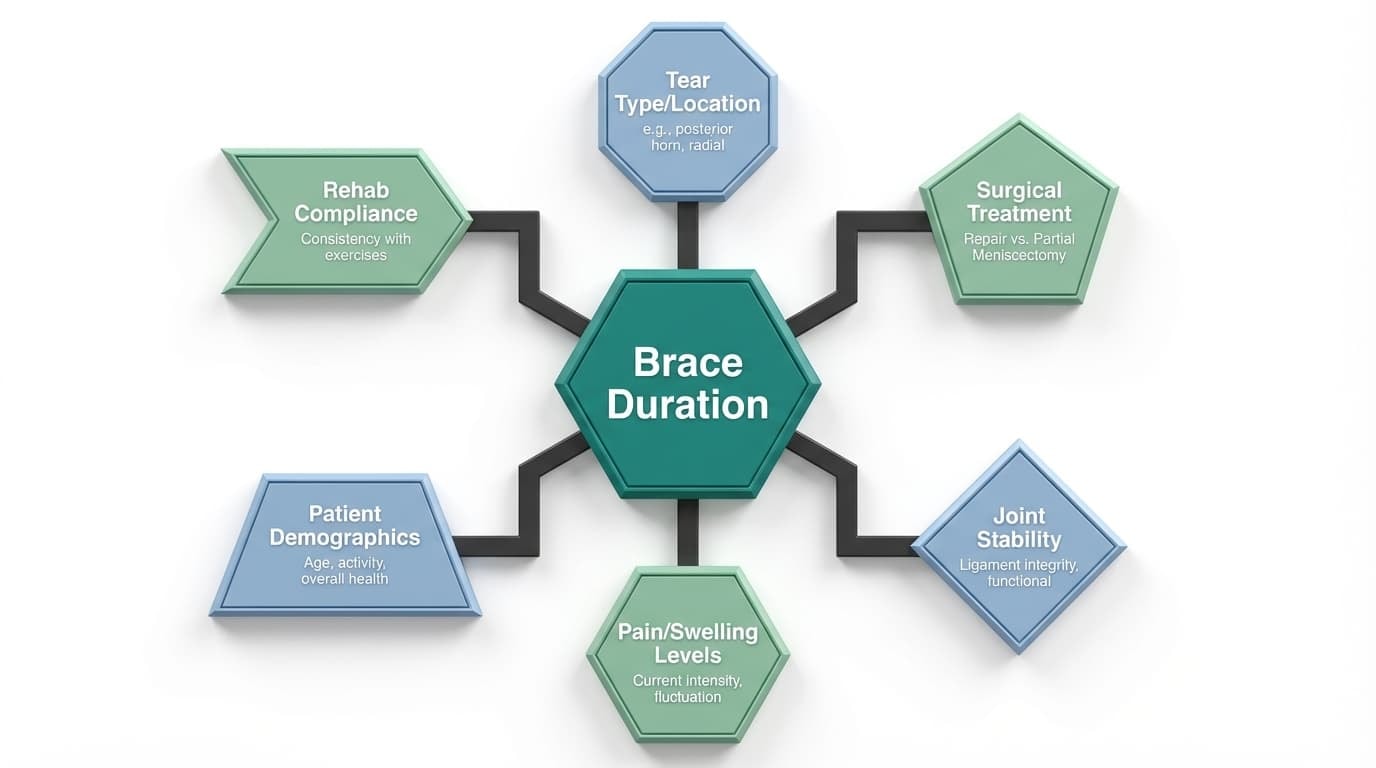
There’s no single timeline for wearing a knee brace after a torn meniscus, because your recovery depends on your unique situation. Your orthopedic surgeon and physical therapist will base your plan on several key factors and adjust it as you heal.
Here’s what matters most:
-
The type and location of your meniscus tear, such as vertical, radial, or complex
-
Whether your meniscus was surgically repaired or partially removed
-
How stable your knee joint is, especially if you also have an ACL injury
-
Your current levels of pain and swelling
-
How consistently you follow your rehab instructions
For example, a clean tear in a well-vascularized area may heal faster. But a root tear, which affects how the meniscus handles joint pressure, often requires longer bracing and stricter protection.
Your therapist will also look at how your knee is responding to rehab. Are you regaining motion? Is swelling under control? Are your quadriceps activating well? These signs help guide when it’s safe to reduce brace use or when you need more time to protect healing tissue.
Most people have follow-up assessments around weeks 2, 6, and 12. These appointments help your provider adjust brace settings, weight-bearing levels, and wear time to keep your knee supported without becoming overly stiff or weak.
Your Surgeon’s and Physical Therapist’s Recommendations
Your surgeon’s protocol is based on what they saw during your procedure, including the tear type, tissue condition, and technique used. It gives your care team a starting point for safe bracing timelines.
From there, your physical therapist customizes the plan based on your progress. They’ll assess your range of motion, swelling, muscle strength, and walking pattern to fine-tune your brace use.
If you skip steps or remove the brace too soon, your risk of reinjury goes up. Studies show that people who stick to their bracing instructions have a 91 percent success rate, while those who don’t see much lower outcomes.
On the flip side, overusing a brace for too long can also delay your recovery. Muscle atrophy can begin within just a few weeks of reduced activity, especially in the quadriceps. Stiffness in the joint, known as arthrofibrosis, is another risk when bracing continues longer than necessary.
To avoid these pitfalls, keep a copy of your brace instructions handy. Take a photo or write them down so you can refer back easily. Clear communication with your care team will keep your recovery on track.
Brace Duration by Meniscus Tear Type and Treatment
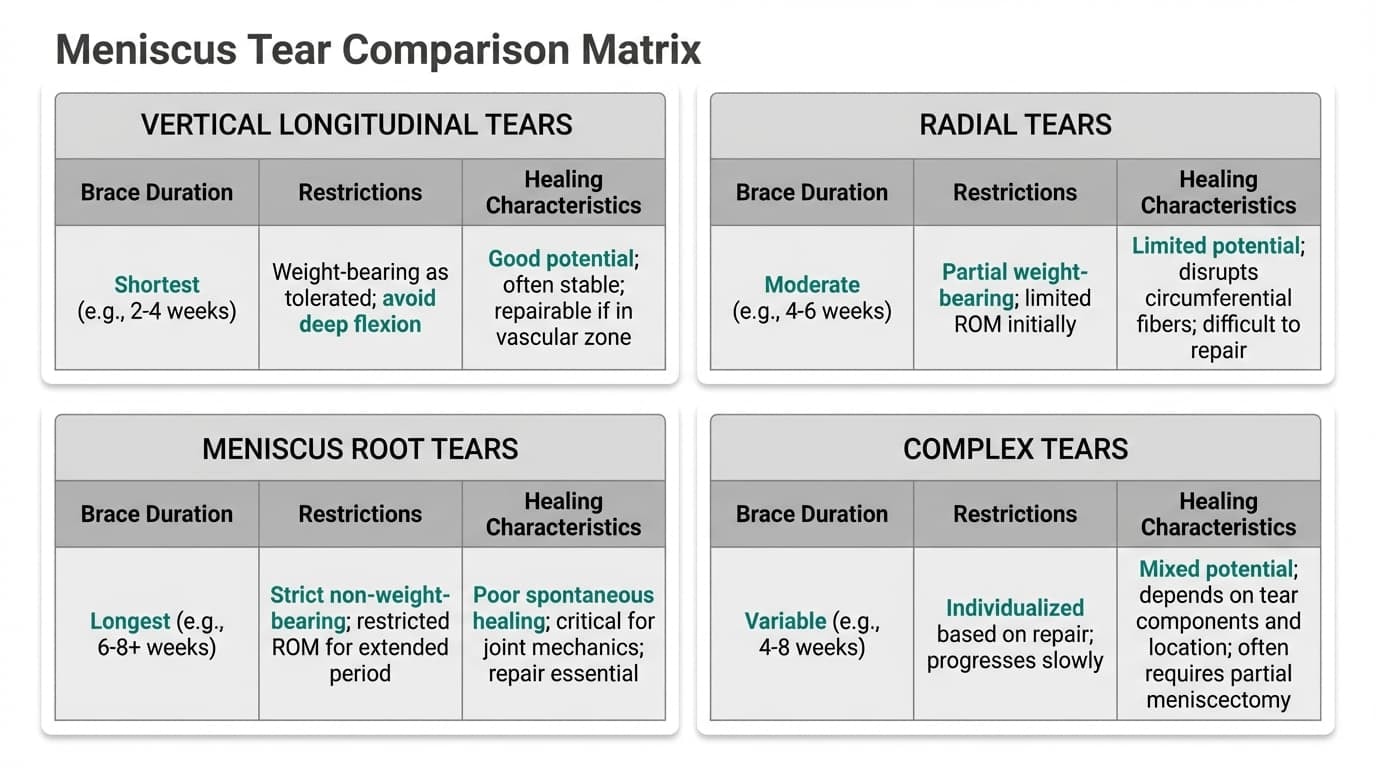
Not all meniscus tears heal the same way, and that is why brace timelines can look very different from one person to another. The location of the tear, its stability, and whether surgery was performed all determine how long your knee needs extra protection.
Understanding your tear type helps you know why your brace is required and how long it should realistically stay on during your recovery journey.
Vertical Longitudinal Tears and Vascular Healing
Vertical longitudinal tears occur along the length of the meniscus and are often located in the outer vascular zone, where blood supply is strongest. Because of this, they have some of the highest healing rates, usually reaching 80-96% when repaired correctly.
Most patients wear a hinged brace for about 6 weeks. Early on, knee bending is limited to protect the stitches from rotational stress. Flexion is commonly restricted to 90 degrees, especially during walking and sitting transitions.
During the first two weeks, the brace provides stability while the body begins forming collagen at the repair site. Around week two, therapists often begin controlled unlocking as strength and swelling improve. The brace remains essential during walking because twisting forces can silently damage the repair even when pain feels minimal.
This structure allows safe motion without risking further damage during early healing.
Radial Tears
Radial tears cut across the meniscus fibers that typically distribute body weight through the joint. Because these fibers do not heal well without protection, bracing becomes critical.
Most radial tears require:
-
A hinged brace worn for 4 to 6 weeks
-
Limited range of motion, often 0 to 90 degrees
-
Reduced or non-weight-bearing early in recovery
These tears are particularly sensitive to loading. Without brace support, compression forces can pull the tear apart before healing occurs.
When a radial tear is combined with an ACL injury, which occurs in nearly half of cases, brace wear often extends to 6 weeks to synchronize ligament and meniscus healing.
The brace limits movement that creates shear stress and protects the knee while stability gradually returns.
Meniscus Root Tears
Root tears are the most serious meniscus injuries and require the strictest brace protocols.
The meniscus root anchors the cartilage to the bone. When it tears, the meniscus loses its ability to absorb force.
Because of this risk, root repair protocols usually include:
-
Brace locked in full extension for walking
-
A brace is worn during sleep
-
Strict non-weight bearing for about 6 weeks
-
Range of motion is only under the therapist's supervision
Most patients continue brace use for 9 to 12 weeks in total. Even after weight bearing resumes, additional support is often needed while strength rebuilds.
Skipping or shortening brace use after root repair significantly increases the risk of repair failure and early osteoarthritis.
Horizontal and Cleavage Tears
Horizontal and cleavage tears are often degenerative and occur from long-term wear rather than sudden trauma. These tears are common in adults over 40 and are frequently associated with early joint changes.
If repaired, brace use is usually brief, often 0 to 4 weeks. Many of these tears are instead treated with a partial meniscectomy, in which damaged tissue is trimmed rather than repaired.
In those cases:
-
Some patients do not need a brace at all
-
Others use a brace for 1 to 2 weeks for comfort
-
Support is mainly used during walking or standing
The brace in this situation does not protect stitches. Instead, it helps reduce discomfort and supports confidence while mobility returns.
Complex Tears
Complex tears involve multiple tear patterns simultaneously and often occur alongside other common knee injuries.
Because stability is compromised in multiple directions, bracing is typically required for 4 to 6 weeks. These injuries also carry a higher re-tear risk, mainly if early twisting occurs.
Patients with complex tears often follow longer rehabilitation timelines of 6 to 9 months. The brace plays a key role early by limiting movement that could overload healing tissue while physical therapy rebuilds muscle control.
Compliance during this phase strongly influences long-term outcomes.
Conservative Non-Surgical Management
Not every torn meniscus requires surgery. Small, stable, or degenerative tears can often heal with conservative treatment that includes physical therapy, activity modification, and strategic brace use.
In non-surgical recovery, the brace is not worn all day. Instead, it provides targeted support during higher stress activities such as:
-
Long walks
-
Stair climbing
-
Work duties
-
Light sport participation
A typical pattern looks like this:
-
Weeks 1 to 2: brace during most daily activities
-
Weeks 3 to 4: brace for walking and work tasks
-
Weeks 5 to 6: brace only for higher demand movement
-
Weeks 6 to 8: tapering to occasional use
The goal is to provide stability without limiting blood circulation or muscle activation. Wearing a brace for too long without strengthening exercises can slow recovery.
For patients needing reliable support during this stage, a well-fitted option like the Anaconda Knee Brace can provide stability while allowing natural movement. It is designed for daily comfort and controlled motion and may be worth discussing with your healthcare provider if you need ongoing activity support.
After Partial Meniscectomy
Partial meniscectomy removes damaged tissue rather than repairing it, which significantly shortens brace requirements.
Most patients:
-
Do not require a brace at all
Brace use beyond the first few weeks is usually unnecessary unless instability or swelling persists. Long-term recovery focuses on restoring strength, improving joint mechanics, and protecting the knee during physical activity.
While osteoarthritis risk may increase years later, prolonged brace use does not prevent this. Strength training, proper movement patterns, and maintaining a healthy body weight play a far larger role.
Phase-by-Phase: How Long and How Often to Wear the Brace (0–12 Weeks)
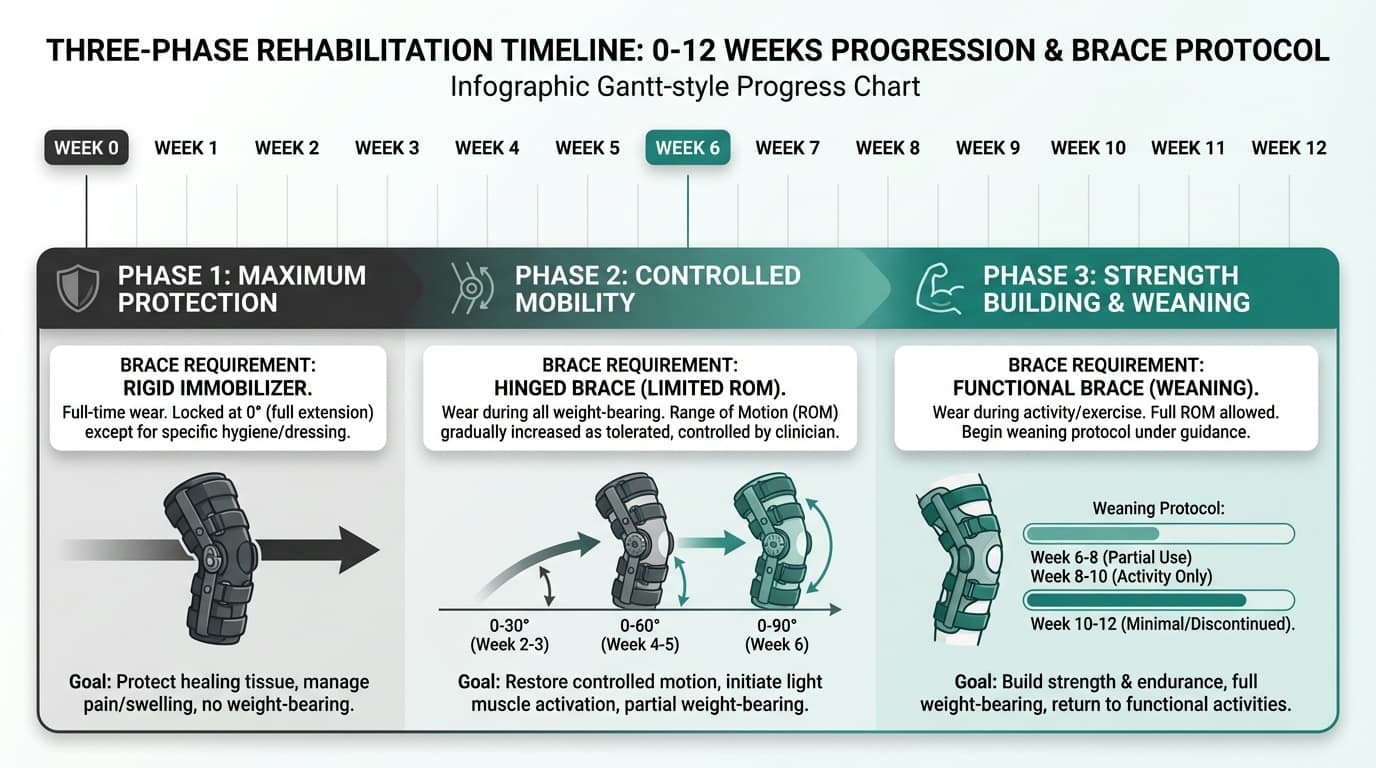
Recovering from a meniscus injury is a gradual process that unfolds in stages. Knowing when and how to wear your knee brace can make all the difference in protecting your healing tissue, reducing pain, and building strength safely. Below is a week-by-week breakdown that outlines what to expect after surgery or during conservative care.
Your brace is not just a piece of gear. It's a tool that helps support joint stability, reduce stress on vulnerable tissue, and guide your knee through each stage of healing. Think of it as a safety net while your body rebuilds.
Before making any significant change in brace use, such as walking without it or sleeping brace-free, get clearance from your surgeon or physical therapist. If you notice increased pain, swelling, or instability, that's a sign to slow down and check in with your provider.
Weeks 0 to 2: Maximum Protection Phase
This is the most restrictive phase of your recovery. The meniscus is highly sensitive to stress, and early healing relies on keeping the joint stable and extended.
During this phase, your brace is typically:
-
Locked in full extension (0 degrees) for walking and resting
-
Worn 24 hours a day, including during sleep
-
Only removed for hygiene, skin checks, or supervised therapy
Weight-bearing is limited. Most patients use crutches and are either toe-touch or partial weight-bearing, depending on the type of surgery. Root repairs usually require strict non-weight-bearing to avoid damaging the meniscal attachment.
Physical therapy during this stage focuses on:
-
Gentle range-of-motion exercises out of the brace, often within 0 to 60 degrees
-
Quadriceps activation without stressing the joint
-
Managing swelling and pain with elevation and ice
Tips for a smoother experience:
-
Use a body pillow to limit movement during sleep
-
Check skin daily for redness, pressure marks, or irritation
-
Keep the brace clean and dry to avoid skin issues
-
Learn how to reapply straps correctly to maintain comfort and blood circulation
Weeks 2 to 6: Controlled Mobility Phase
Once initial healing has started, the focus shifts to carefully restoring motion and allowing light loading. The brace is still essential, but its settings begin to change.
What usually happens in this phase:
-
The brace is gradually unlocked to allow 60 degrees of motion by week 2 or 3
-
Progresses to 90 degrees of flexion by weeks 4 to 6
-
Weight-bearing typically increases as tolerated by week 4
-
Nighttime brace wear may be discontinued after week 2 (unless advised otherwise)
This is a critical time. The meniscus may feel better, but it's still fragile. Avoid high-load activities, fast movements, or uneven surfaces. The brace helps prevent unintended twisting or bending that could compromise healing.
Patients who had ACL reconstruction, complex tears, or delayed muscle activation may need to stay in the locked or partially restricted brace longer. Always follow your provider’s instructions closely.
Weeks 6 to 12: Strength Building and Weaning Phase
By this point, healing is well underway. Now it’s time to shift away from brace dependency and gradually rebuild functional strength. The brace moves into part-time use based on your activity level.
Typical progression looks like:
-
Short, supervised walking indoors without the brace starting around week 6
-
Transitioning to full days at home without it between weeks 7 and 9
-
Wearing the brace only during high-risk activities like stairs, busy environments, or exercise
This is also when some patients switch to a lighter brace or an unloader knee brace for activities that involve more motion. These options still provide support and compression without the bulk of post-operative bracing.
You're generally ready to reduce or remove the brace when you can:
-
Walk with a symmetrical gait and no limp
-
Perform a straight-leg raise without knee lag
-
Stand on your operated leg without wobbling
-
Achieve near-full range of motion (ideally 120 degrees or more)
-
Complete basic activities with minimal swelling
By week 12, many patients are brace-free for most daily tasks. However, clearance for high-impact sports, pivoting, or contact activities often comes later, depending on your specific injury and progress in rehab.
How Daily Life Affects How Long You Wear Your Knee Brace
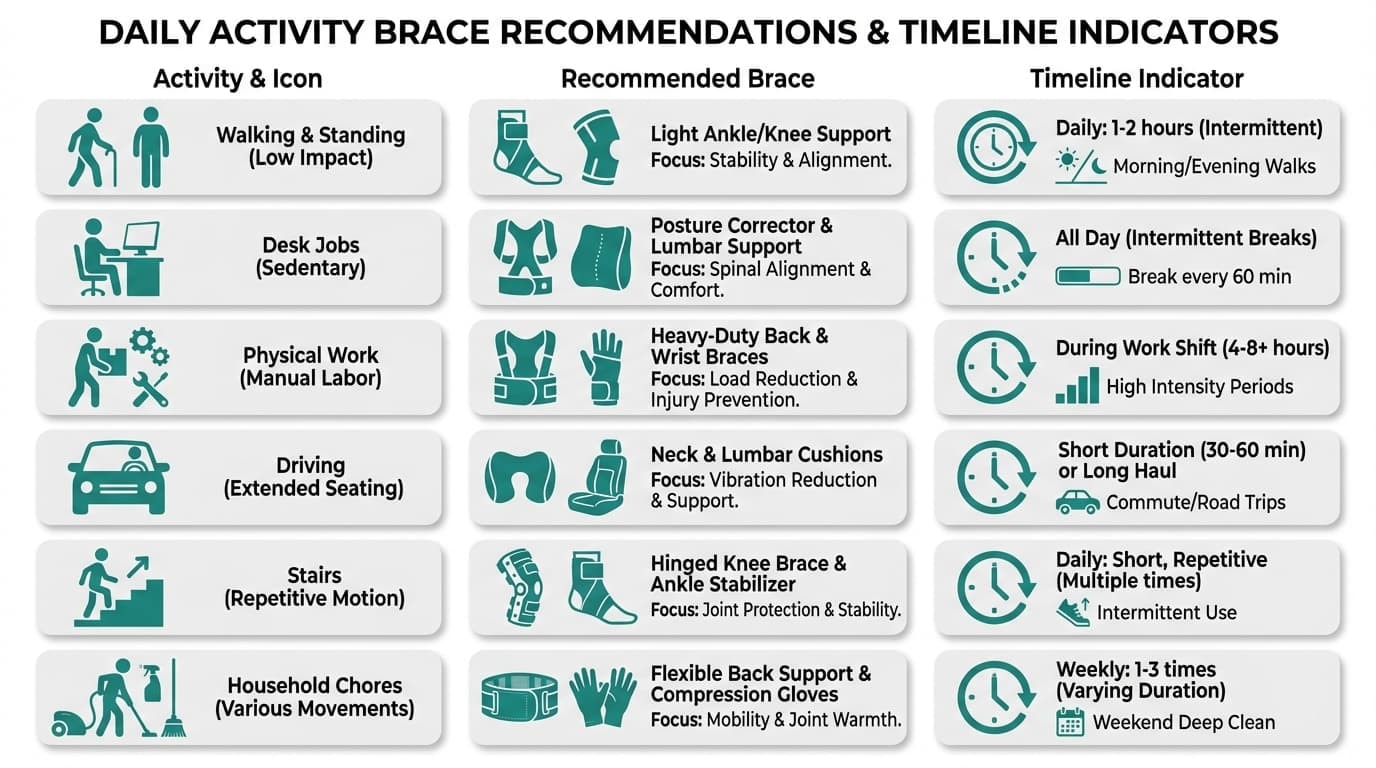
How long you need to wear a knee brace isn’t just about your injury or surgery. Your day-to-day activities play a significant role. Everything from your job and sleep habits to how much you walk or stand can affect your brace schedule and healing speed.
Let’s look at how different lifestyle factors influence brace use and how to adjust safely without risking healing.
Walking and Standing
Even routine walking puts pressure on a healing meniscus. During the first four weeks, you should wear a knee brace any time you’re walking outside your home. For indoor walking, most physical therapists recommend continued brace use through the early recovery phase to provide stability and prevent strain.
Longer walks, shopping trips, or standing for extended periods increase joint stress. Keep your brace on during these tasks until your physical therapist clears you to go without it.
Desk Jobs vs. Physical Work
If you work a desk job, you may be able to reduce brace use earlier, especially if you're mostly sitting. Just be mindful when standing or moving around the office.
For those with manual labor jobs, such as construction, warehouse work, or caregiving, brace use often extends longer. These jobs require squatting, bending, climbing, and carrying weight, which can put the knee under high stress. Talk to your healthcare provider about temporary work restrictions or modified duties to prevent setbacks.
Driving
Driving after knee surgery is a milestone, but it must be approached safely. If your surgery was on the right leg, driving is usually restricted for several weeks. You need complete muscle control, pain-free movement, and fast reaction time to brake or accelerate without hesitation.
Never resume driving without your doctor's or physical therapist’s approval. The type of knee brace you need may also impact pedal control, especially if you're wearing a hinged knee brace that limits motion.
Using Stairs
Stairs create more joint compression than walking on flat ground. That’s why most providers advise continued brace wear when using stairs, even after you’ve started walking unbraced indoors.
Generally, stairs call for extra caution until around weeks six to eight. Step carefully and use a railing whenever possible.
Household Chores
Cooking, cleaning, and laundry may seem harmless, but they involve frequent bending, twisting, and turning, all movements that can irritate healing tissue. Wear a knee brace for these activities until cleared by your provider, and avoid kneeling or squatting altogether.
If you’re experiencing discomfort or instability while doing chores, your brace may need adjustment. The Anaconda Knee Brace is an excellent option for this phase, offering targeted support that stays comfortable during daily use.
Travel and Transitions
Planning a trip or returning to work? Time it around key follow-up visits. Your physical therapist can reassess your joint, review your range of motion, and provide updated guidance on brace use for travel or commuting.
Even if your knee feels normal, that doesn’t always mean it’s fully healed. Internal tissues take time to rebuild. Always base your brace-weaning timeline on professional clearance, not just comfort.
Wearing Your Knee Brace at Night and During Rest
Bracing at night may seem unnecessary, but for certain surgeries and tear types, it’s a critical part of the healing process. Sudden movements during sleep can stress vulnerable structures and delay recovery.
Why Night Bracing Matters
In the first few weeks after surgery, especially following a meniscus root repair, wearing a knee brace at night helps keep your joint stable while you sleep. It prevents accidental bending or twisting that could damage the repair or trigger pain.
Most patients continue wearing a knee brace during sleep until weeks two to six. The exact timeline depends on:
-
The type of meniscus tear or whether you had an anterior cruciate ligament repair
-
Your surgeon’s specific protocol
-
How well you can stay in a safe sleep position
Root repairs often require the longest nighttime support, sometimes for six weeks or more.
Struggling to Sleep in Your Brace?
Nighttime bracing can be uncomfortable at first, but a few strategies can help reduce stress and improve sleep quality:
-
Place a pillow under your braced leg to minimize pressure
-
Sleep on your back to avoid twisting your knee
-
Use a body pillow to keep you from rolling
-
Check for tightness to ensure good blood circulation
-
Wear a breathable knee sleeve underneath the brace to reduce friction
If your brace causes ongoing discomfort or you notice tingling or numbness, call your doctor or physical therapist. A slight adjustment may restore comfort without compromising safety.
The Anaconda Knee Brace is designed for all-day and night wear. Its breathable materials and adjustable straps help reduce discomfort, making it a good fit if you need continuous support during your recovery journey.
Risks of Wearing a Knee Brace Too Long or Not Long Enough
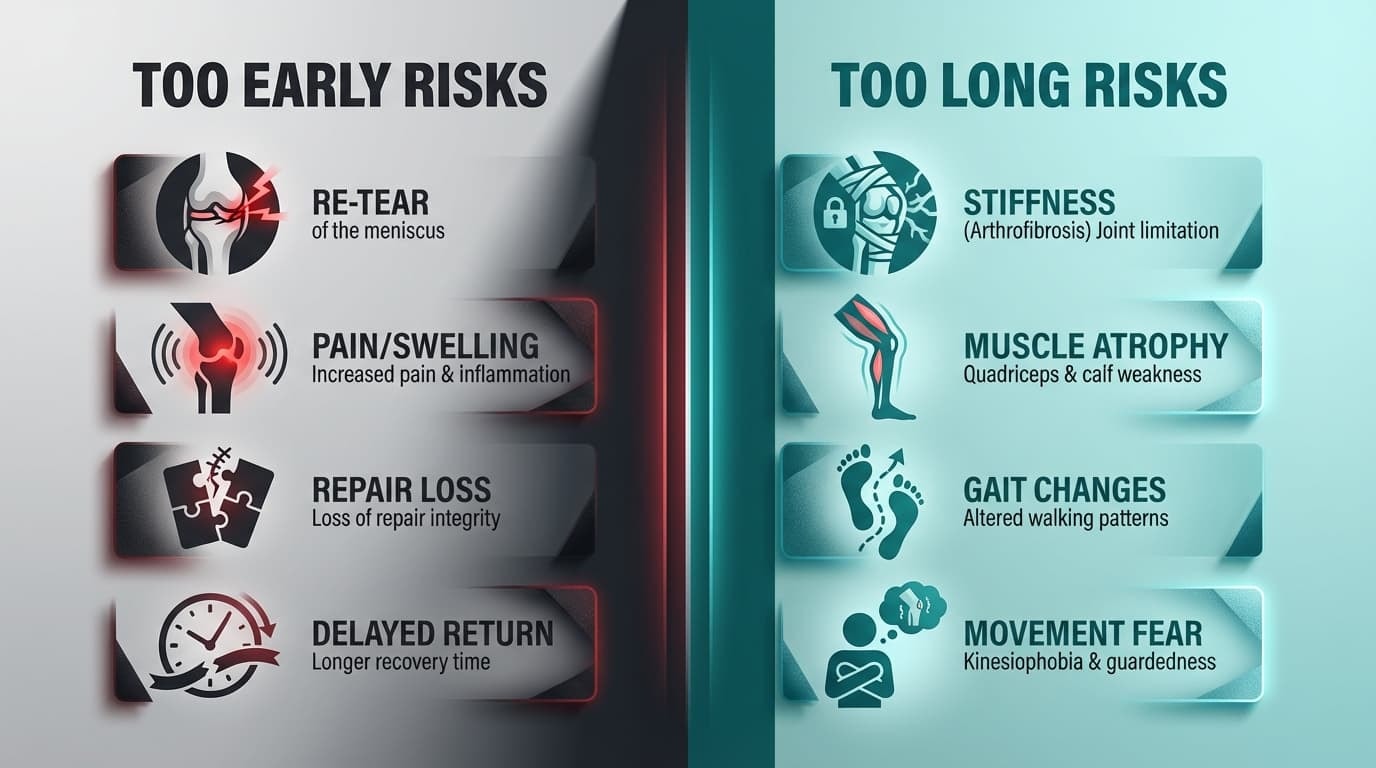
Wearing a knee brace can be a key part of healing from a torn meniscus or other knee injuries, but timing matters. You need to wear it long enough to protect the healing tissue and provide support, but not so long that it harms your joint function or muscle strength.
This balance point depends on your condition, treatment, and progress. That’s why it’s so important to follow your healthcare provider or physical therapist’s guidance.
Risks of Stopping Brace Use Too Early
If you take off your brace too soon, you could slow down healing or even undo the progress you’ve made. The first six weeks after knee surgery are often the most critical, especially if you had a hinged knee brace placed after a repair.
Possible consequences include:
-
Re-tear of the meniscus: The repaired tissue may not be strong enough yet and could fail, requiring another surgery.
-
Increased pain and swelling: Premature removal can lead to inflammation and irritation in the healing area.
-
Loss of repair integrity: You may end up needing a partial meniscectomy if the tissue cannot heal properly.
-
Delayed return to sports or work: An early setback can add weeks or months to your recovery journey.
Even if your knee feels better, that doesn't mean the tissue is fully healed. It is essential to complete the full recovery process under medical supervision.
Risks of Wearing a Knee Brace Too Long
On the other hand, keeping the brace on too long can lead to long-term problems. Immobilizing the knee for several weeks without proper weaning or therapy may create new challenges.
What might happen if you keep wearing the brace too long:
-
Joint stiffness (arthrofibrosis): The knee can lose range of motion if not gradually reintroduced to movement.
-
Quadriceps and calf muscle atrophy: Without use, your muscles weaken quickly, especially during reduced physical activity.
-
Altered gait patterns: Compensating for knee weakness can strain the hips, back, or other joints.
-
Fear of movement: Some people become dependent on the brace, which can hold back their confidence in their own stability.
You may also notice skin irritation, discomfort, or reduced blood circulation if the brace is too tight. Tingling or numbness around the knee or lower leg may signal nerve pressure and should be addressed immediately.
How to Know When It’s Safe to Reduce Brace Use
You and your physical therapist will decide together when to begin tapering off your brace use. This should be based on both clinical signs and how your knee feels and functions during daily activities.
You may be ready to reduce brace time if you can:
-
Walk indoors without limping
-
Perform straight-leg raises without knee lag
-
Stand steadily on the operated leg
-
Climb stairs using only light hand support
-
Move through your day with minimal swelling or pain
Your provider will also check for:
-
Full or near-full extension of the knee
-
Flexion that continues to improve beyond 120 degrees
-
Solid quadriceps control
-
Good balance and body awareness
Keep in mind that being ready means your knee has healed enough and that you’ve built the strength to move safely. Start tapering in controlled environments, such as indoors, before removing the brace for outdoor or demanding tasks.
Never change your brace schedule on your own. Always consult your doctor or therapist before adjusting wear time, unlocking settings, or changing weight-bearing levels.
If you are transitioning out of a rigid post-op brace and still need some additional support, an unloader knee brace or a soft compression sleeve may provide the right amount of control and flexibility. If you’re unsure which knee brace you need, ask your provider for a recommendation based on your progress.
For those who need both structure and comfort, the Anaconda Knee Brace offers excellent support during rehab and return to activity. Talk to your clinician about whether it’s the right fit for your recovery stage.
Practical Tips for Using a Knee Brace During Meniscus Recovery
Wearing a knee brace during meniscus recovery is not just about strapping it on and going about your day. Small but important details in how you wear, adjust, and care for your brace can make a major difference in your recovery process and help prevent long-term problems.
Whether you're recovering from ACL reconstruction or meniscus surgery, or managing a knee injury without surgery, these practical strategies will help you stay comfortable, protect your healing joint, and get the most benefit from your brace.
1. Fit Matters: Correct Sizing and Strap Adjustment
Your brace should fit securely and align its hinges with the natural bend of your knee. It should not slide down, pinch, or cause skin breakdown. Straps need to be snug enough to provide stability, but not so tight as to restrict blood circulation or cause numbness.
Check your fit every day, especially after showering or extended wear. If you feel tingling, cold toes, or unusual tightness, loosen the straps and consult your healthcare provider.
Pro tip: Have your doctor or brace fitter walk you through proper strap tension and reapplication during your first fitting.
2. Wear a Thin Layer Underneath
To prevent discomfort, chafing, and skin irritation, wear a knee sleeve or a thin, moisture-wicking compression layer under your brace. This barrier helps reduce pressure points and absorb sweat during long wear, especially in warm climates or active settings.
Make sure the layer doesn’t bunch under the straps, as this could limit movement or create uneven stress on the skin.
3. Do Daily Skin Checks
Inspect your skin at least once a day, ideally when you remove the brace for hygiene or physical therapy. Look for:
-
Redness or hot spots
-
Blisters or open areas
-
Indentations or tight marks from straps
Most minor issues resolve with a break and repositioning, but persistent skin problems may signal a poor fit. If issues continue, bring them up at your next doctor or physical therapist visit.
4. Combine Brace Use With Complete Rehab Care
A knee brace is not a substitute for physical activity or muscle strengthening. To make real progress, it needs to be part of a larger plan that addresses strength, flexibility, and tissue healing.
Combine your brace with:
-
Daily physical therapy exercises tailored to your injury
-
Icing and leg elevation to control swelling and pain
-
Adequate rest to allow healing
-
Nutritious meals that support tissue repair and joint health
If you rely solely on your brace without working to rebuild strength, you may develop muscle atrophy or lingering joint weakness that could lead to future problems.
5. Don’t Ignore Red Flags
Contact your healthcare provider or physical therapist immediately if you experience:
Serious symptoms:
-
Sharp or sudden pain in the knee
-
A popping or tearing sensation
-
Locking, catching, or instability when walking
-
Swelling that worsens quickly
-
Inability to bear weight despite being cleared to do so
Brace-related complications:
-
Skin breakdown or visible sores
-
Persistent numbness or tingling below the brace
-
Cold, blue toes
-
Inability to move your ankle or toes normally
These signs may indicate that your brace needs adjustment, that your activity level is too high, or that there’s a complication that requires imaging or a change in your recovery plan.
6. Bring Your Brace to Every Appointment
Your care team may adjust your brace settings over time, especially as you transition from restricted movement to more active rehabilitation. Always bring your brace to follow-up visits so your provider can:
-
Check alignment and hinge angle
-
Assess wear-and-tear
-
Demonstrate new positions for walking or sleeping
-
Evaluate whether you’re ready to switch to a lighter brace or knee sleeve
Regular check-ins help prevent small issues from becoming serious problems and support a smoother healing journey.
Final Thoughts
Wearing a knee brace properly is about more than protection; it’s about being proactive in your recovery. The right fit, daily care, and innovative use can provide support, enhance comfort, and minimize risk as you regain knee stability.
If you’re looking for a brace that’s built for both comfort and performance, the Anaconda Knee Brace offers customizable fit, breathable design, and reliable joint control through every stage of your recovery journey. Ask your provider if a knee brace is what you need for lasting results.
By following these tips, you can move through the next several weeks of healing with confidence, clarity, and control.
FAQs
Quick answers to the most common questions about knee braces and torn meniscus recovery.
Can I walk without my knee brace at home if my knee feels okay?
Walking without your knee brace should only start when your physical therapist or surgeon says it’s safe. Feeling okay doesn’t mean the meniscus tear has fully healed. Most people wait until around week 6 after knee surgery, depending on the type of torn meniscus. Always follow medical advice to avoid reinjury.
Do I need to wear my knee brace while exercising in physical therapy?
Yes, you usually need to wear a knee brace during early physical therapy exercises. Some movement exercises may be performed outside the brace, but only under direct supervision. Weight-bearing exercises often require a hinged knee brace to support the healing knee joint. Your physical therapist will tell you when it's safe to remove it.
Is it safe to drive while wearing a knee brace after a meniscus tear?
Driving after a meniscus injury is only safe when you can fully control the pedals. For a right-leg meniscus tear, this may take several weeks. A knee brace can restrict reaction time, especially after knee surgery. Get your doctor's clearance and test in a parked car before driving.
Will I always need a knee brace for sports after my meniscus heals?
You won’t always need a knee brace after your torn meniscus heals. Athletes with prior knee injuries or anterior cruciate ligament issues may benefit from using a hinged brace or unloader knee brace. This can help prevent injuries during high-demand activity. Talk with your surgeon about sport-specific options.
What if my brace is uncomfortable or causing pain?
If your knee brace is causing discomfort, check the strap tightness and hinge alignment. A knee sleeve underneath can reduce rubbing and improve comfort. Don’t stop using the brace without your physical therapist's or provider's advice. Wearing it incorrectly may worsen your condition or delay healing.













![How Long Should You Wear a Knee Brace? [Ultimate Guide to Maximize Recovery]](http://anacondafightwear.co/cdn/shop/articles/How_Long_Should_You_Wear_a_Knee_Brace_26a1ef4d-6a7f-4b6f-9499-d5e24daf9626.jpg?v=1769715635&width=533)
